Calcinosis Cutis on Vulgar Wart. Report of a Case
Abstract
Verruca vulgaris is a very common lesion, of viral etiology, benign clinical behavior and different types of simple treatments. Its epidemiological, morphological, histological and therapeutic study has been sufficiently reflected in the literature. We present a peculiar clinical case in which calcium deposits developed on a common wart without any alterations in its metabolism being observed in the analytical studies carried out (calcinosis cutis). A 9-year-old male patient attended the dermatology service due to an excrescent keratotic lesion of recent appearance and rapid growth. We have conducted an unsucessful bibliographic search of this relationship, possibly because these have not been communicated because it is simply a morphological finding with no clinical significance.
Author Contributions
Copyright © 2022 Francisco Javier Torres-Gómez
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Verruca vulgaris is a very common lesion, of viral etiology, benign clinical behavior and different types of simple treatments. Its epidemiological, morphological, histological and therapeutic study has been sufficiently reflected in the literature. We present a peculiar clinical case in which calcium deposits developed on a common wart without any alterations in its metabolism being observed in the analytical studies carried out (calcinosis cutis). A 9-year-old male patient attended the dermatology service presenting with an excrescent keratotic lesion of recent appearance and rapid growth. We conducted an unsuccessful bibliographic search of this relationship, probably because these have not been communicated because it is simply a morphological finding with no clinical significance.
Clinical Case
A 9-year-old male patient who was treated in the dermatology service for a progressively growing keratotic nummular dermal lesion on the right knee. With the clinical judgment of viral wart, the lesion was removed. In the Pathology Service, a nummular keratotic lesion of 0.5 cm in maximum dimensions was received, which crackled when cut. Figure 1, Figure 2, Figure 3, Figure 4, Figure 5
Figure 1.Hyperkeratosis, hypergranulosis, proliferation of dermal vessels, and surface and deep calcium deposits. HE. 100x.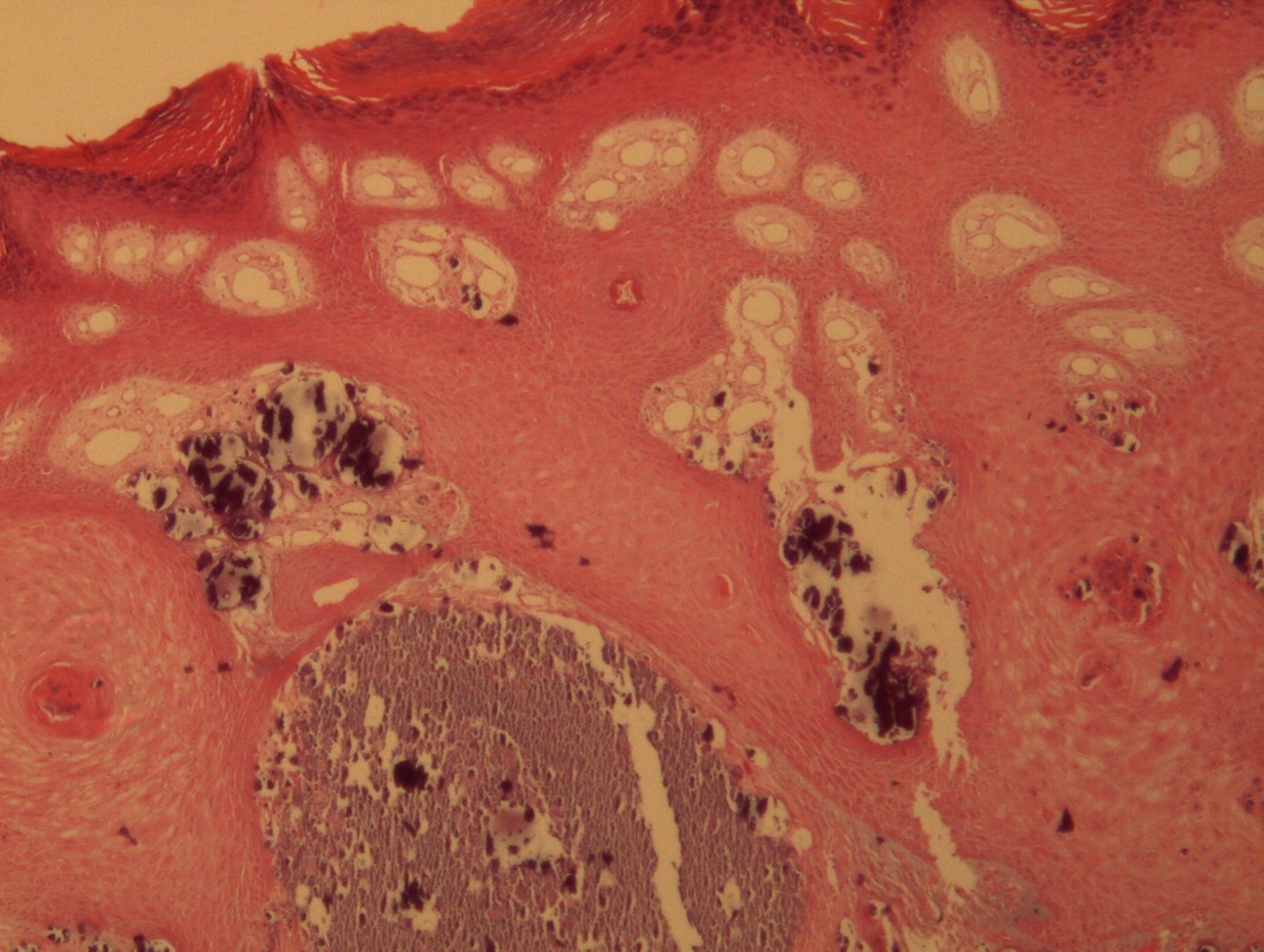
Figure 2.Common wart with calcium foci at the level of the dermal vessels grouped in lobules. HE. 200x.
Figure 3.Relationship of calcium foci in the papillary dermis with the overlying epidermal hyperplasia. HE. 200x.
Figure 4.Presence of calcium deposits in the dermal vessels. Detail. HE 400x.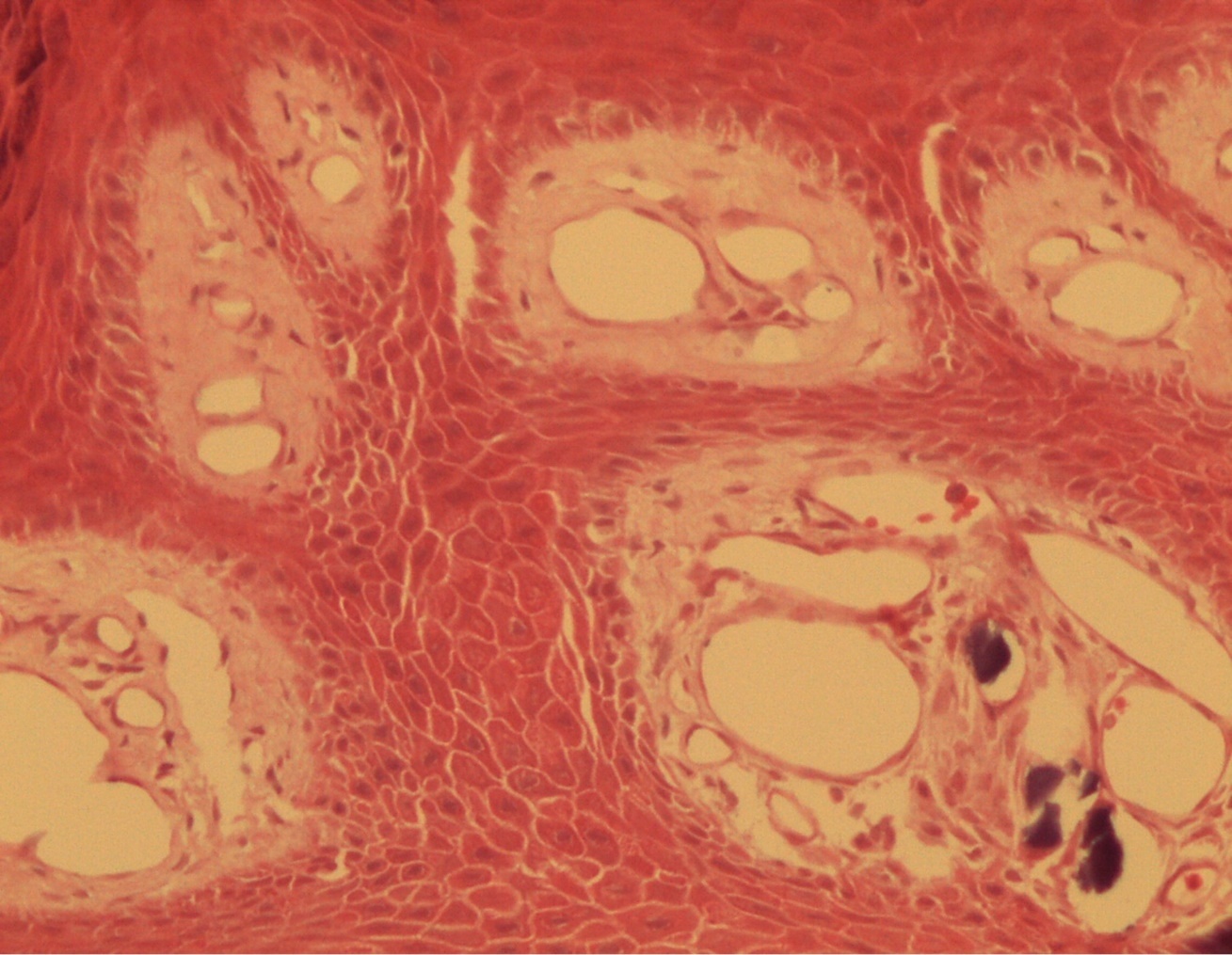
Discussion
Calcinosis cutis refers to the deposit of calcium salts on the skin. It generally constitutes a morphological type of dystrophic calcium deposit, related to different types of lesions or injured tissues (in this case a common wart) without alterations in calcium metabolism in biochemical studies, typical of metastatic calcifications.
The association of both processes and the age of their presentation is striking. We have carried out a bibliographic search without finding cases with the same characteristics. This is probably due to the fact that calcinosis cutis is considered a morphological change or a clinical finding without consequences or diagnostic implications. However, calcinosis cutis has been described accompanying numerous pathological processes 1, 2, 3, 4, 5.
The presence of intralesional calcium deposits is not associated with prognostic consequences. In fact, it is a morphological finding that is anecdotal in most cases. However, it can lead to errors in initial clinical judgement. Depending on its extension and location within the lesion (superficial or deep) it can alter its properties.
At an early age, like that of our patient, it is possible to make wrong clinical diagnoses, mainly that of pilomatricoma, a lesion with which it is necessary to make a clinical, but not histological, diagnosis. It is always advisable to carry out a measurement of calcium levels to rule out other scenarios.
Surgical excision is the appropriate treatment since it is a benign lesion whose behavior is not different from that of a common wart. After eight months of follow-up, no recurrences or foci of calcinosis cutis have been observed in other locations.
References
- 1.Róbert L, Kiss N, Medvecz M, Kuroli E, Sárdy M et al. (2020) Epidemiology and Treatment of Calcinosis Cutis: 13 Years of Experience. Indian. 65(2), 105-111.
- 2.Muddegowda P H, Lingegowda J B, Ramachandrarao R K, Konapur P G.Calcinosis cutis: report of 4 cases. , J Lab Physicians 3(2), 125-126.
- 3.Cohen P R, Tschen J A.Idiopathic calcinosis cutis of the penis. , J Clin Aesthet Dermatol 5(12), 23-30.

