Abstract
Purpose:
The aim of the study was to analyze the spatial relationship between the sinus floor and the alveolar bone of maxillary premolars and molars in order to assess the amount of basal bone available for immediate extraction placement of endosseous implants.
Materials and Methods:
All the cone-beam computerized tomographic (CBCT) scans taken over a three-year period at four centers were identified. The subsinus bone height (SBH) was evaluated by measuring the distance between the sinus floor and the first and second premolar root apexes. The interradicular septum bone height (ISBH) of all the first and second molars was also measured, and the presence or absence of sinus-floor invagination between the molar roots was recorded.
Results:
Five hundred twenty-six (526) CBCT scans of fully or partially dentate maxillary arches were examined. The root apex was inside the sinus of 1.8% of all the first premolars. It approximated the sinus floor of 5.3% of them, and the distance between the two points was between 1 and 3mm of 20%, between 3 and 7mm for 34.1%, and more than 7mm for 34.1%. For the second premolars, the findings were 13.5% (inside the sinus), 10.5% (touching the sinus), 32.8% (1-3mm of distance) 28% (3-7 mm), and 15.2% (more than 7mm). Root invagination was noted in 50.2% of the first molars and 43.1% of the second molars, with the ISBHs ranging from 13.4% to 56.9%. Conclusion: Radiological evaluation is essential to determining whether implants should be placed immediately after extraction of maxillary premolars and molars.
Author Contributions
Academic Editor: Janet H. Southerland, Meharry Medical College Department of Oral and Maxillofacial Surgery Meharry Medical College School of Dentistry
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Francesco Amato
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Although the use of osseointegrated implants to replace missing teeth has become a predictable procedure with high implant survival rates 1, 2, success rates in the posterior maxilla are lower due to the poor quality and inadequate height of bone.3 Furthermore, after tooth loss, the periosteum of the maxillary sinus can exhibit increased osteoclastic activity, which can cause bone resorption 4 and a resumption of the physiological sinus- floor pneumatization process.5, 6 The result is a progressive reduction of the bone height. Subsinus alveolar bone height (SBH) has been defined as the distance between the floor of the maxillary sinus and the alveolar crest.7 A lack of SBH may be treated in different ways depending on the degree of atrophy. Options include sinus lift augmentation, vertical bone regeneration of the alveolar ridge, interpositional grafting, short implants, or use of alternative sites (tuberal, pterygoid, zygoma, or tilted).8, 9, 10 A valid alternative to prevent post-extraction sinus-floor pneumatization and avoid the need for grafting procedures can be immediate extraction implant placement.
Several authors have advocated that one of the main criteria for achieving good primary stability with implants immediately placed in extraction sites is to engage the implant in the bone apical to the root apex.11, 12, 13 When taking this approach, however, it is essential to be aware of the amount of basal bone and the relationship between the root apex and the anatomical landmarks apical to it: the nasal floor and the anterior part of the sinus floor for the premolars and the posterior portion of the sinus floor and interradicular bone septum height for the molars.
SBH has been investigated by several authors7, 14, 15, 16 using panoramic radiographs of edentulous maxillae. Other authors have used three-dimensional diagnostic tools to gather anatomical information about this area.17, 18, 19, 20, 21
The aim of this retrospective study was to further investigate the relationship between the alveolar bone available for implant insertion and the anatomical structures located apical to it in the maxillary premolar and molar area, including the interradicular bone septum height (IBSH) in the molar area. The goal was to create clinical guidelines so that dentists can better avoid sinus perforation at the time of extraction followed by immediate implant placement in the posterior maxillary area.
Material and Methods
All the cone-beam computerized tomographic (CBCT) scans of patients with fully or partially dentate maxillary arches that were taken over the previous three years were identified at a private dental practice in Catania, Italy, as well as at three different radiology centers. The scans were obtained using several different machines (Gendex CB-500, NewTom Vgi, Toshiba Aquilon 64 TSX-101A, Soredex Scanora 3D Conebeam, Planmeca ProMax 3D, and Siemens Somaton). The CBCT scans, previously done for various diagnostic purpose, were included in the study only if a correct calibration of the machine was been performed. The data were collected from April 2014 to October 2014. Prior to start the measurement, the calibration of the system was controlled. The same operator, three times for each landmark, took all the measurements. A mean value of the three measurements was carried out. On the basis of the obtained value, all the tooth were distributed in the corresponding Group. A percentage value of the distribution of the teeth in the corresponding Group was carried out.
Patients inclusion criteria were the following:
1. The patients scanned had to be 18 years or older.
2. At least two maxillary posterior teeth had to be present on each side.
3. No impacted teeth or other pathology could be present in the posterior maxillary alveolar bone.
4. Patients could be either non-smokers or smokers.
On each scan, the anatomical relationships were measured using each machine’s respective dedicated software (V3.20 R008 Dental MPR, Ondemand 3D, Romexis Viewer, OsiriX Viewer). For each scan, the relationship between the root apex and the nasal or sinus floor was measured for the premolars. In the molar area, the presence of sinus-floor invagination between the roots was evaluated, and the interradicular septum bone height (ISBH) was measured.
Findings for the premolars were classified into five groups, as follows:
1. The root apex was located inside the sinus (Group A)
2. The distance of the root apex from the sinus floor was 0 mm with the root apex, but not penetrating in the sinus (Group B)
3. The distance was 1 to 3 mm (Group C)
4. The distance was 3 to 7 mm (Group D)
5. The distance was more than 7 mm (Group E)
Figure 1 presents examples of each of the five categories.
Figure 1.Classification in five different categories for premolars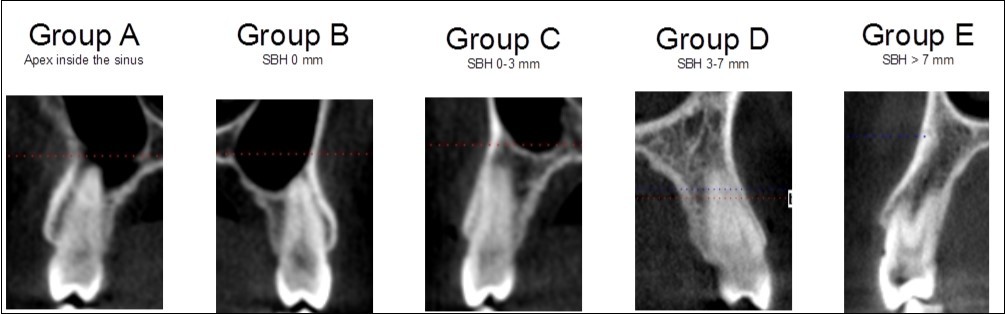
Findings for the molars were classified into two groups, depending upon whether sinus-floor invagination was present between the roots (Group B) or not (Group A) (Figure 2).
Figure 2.Classification in two different categories for molars , based on sinus invagination
The molar findings regarding interradicular septum bone height (ISBH) were further classified into subgroups for each of the two main groups as follows:
1. Subgroup A1: ISBH < 7 mm
2. Subgroup A2: ISBH > 7 mm
3. Subgroup B1: ISBH < 5 mm
4. Subgroup B2: ISBH > 5 mm
Figure 3 presents examples of each of the four categories.
Figure 3.Classification in four different categories for molars, based on sinus invagination and interradicular bone septum height (ISBH). 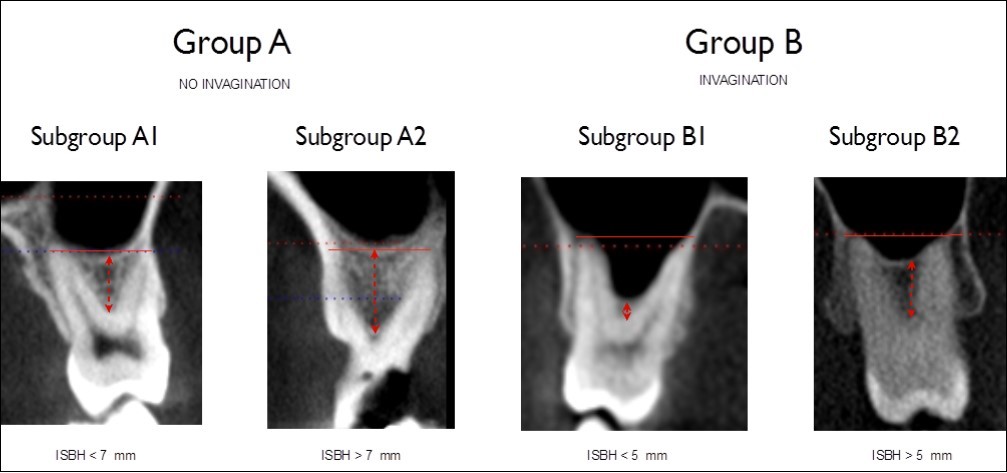
Results
A total of 526 CBCT scans from 278 female and
248 male patients were analyzed. The patients were 18
yo or older (from 19 to 78 yo; mean 46 yo). The scans included 830 first premolars. The root tip of 15 of these (1.8%) protruded inside the sinus (Group A). It was just touching the sinus floor of 44 first premolars (5.3%, Group B). The distance between the root tip and the sinus floor was greater than 0mm and up to 3mm for 166 first premolars (20%, Group C), it was greater than 3mm and up to 7mm for 283 first premolars (34.1%, Group D), and it was more than 7 mm for 322 (38.7%, Group E).
A total of 800 second premolars were analyzed. The root tip of 108 of these (13.5%) protruded inside the sinus (Group A). It was just touching the sinus floor of 84 second premolars (10.5%, Group B). The distance between the root tip and the sinus floor was greater than 0mm and up to 3mm for 263 second premolars (32.8%, Group C), it was greater than 3mm and up to 7mm for 224 second premolars (28%, Group D), and it was more than 7 mm for 121 (15.2%, Group E). Table 1 summarizes the findings for premolars.
Table 1. Premolars Findings| Tooth | Total teeth | Group A SBH<0mm | Group B SBH=0mm | Group C SBH>0-≤3mm | Group D SBH>3-≤7mm | Group E SBH>7 |
| First Premolars | 830 | N=15 1,8% | N=44 5,3% | N=166 20.1% | N=283 34,1% | N=322 38,7% |
| Second Premolars | 800 | N=108 13,5% | N=84 10,5% | N=263 32,8% | N=224 28.0% | N=121 15,2% |
In the molar area, a total of 1,092 first molars were analyzed. No invagination of the sinus floor between the roots was found in 544 (49.8%) of the first molars (Group A). Of these, 146 (13.4%) had an ISBH of less than 7mm (Subgroup A1), while 398 (36.4%) had an ISBH of greater than 7 mm (Subgroup A2). Sinus invagination between the roots was found in 548 (50.2%) of the first molars (Group B). Of these, 260 (23.8%) had an ISBH of less than 5 mm (Subgroup B1), while 288 (26.4%) had an ISBH of greater than 5 mm (Subgroup B2).
A total of 1,108 second molars were analyzed. No invagination of the sinus floor between the roots was found in 630 (56.9%, Group A). Of these, 188 (17%) had an ISBH of less than 7mm (Subgroup A1), while 442 (39.9%) had an ISBH of greater than 7 mm (Subgroup A2). Sinus invagination between the roots was found in 478 (43.1%) of the second molars (Group B). Of these, 169 (15.2%) had an ISBH less than 5 mm (Subgroup B1), while 309 (27.9%) had an ISBH of greater than 5 mm (Subgroup B2). Table 2 summarizes the molar findings.
Table 2. Molars Findings| Tooth | Total teeth | Subgroup A1 No invag ISBH≤7mm | Subgroup A2 No invag ISBH>7mm | Subgroup B1 Invag ISBH≤5mm | Subgroup B2 Invag ISBH>5mm |
| First Molars | 1092 | N=146 13,4% | N=398 36,4% | N=260 23,8% | N=288 26,4% |
| Second Molars | 1108 | N=188 17.0% | N=442 39,9% | N=169 15,2% | N=309 27,9% |
Discussion
The relationship between the premolar and molar roots and the sinus in the maxillary posterior area is complex and has a high individual variability due to the anatomical structure of the sinus. Several factors influence the development of the sinus, including growth, function, and pneumatization. The alveolar dental scaffold, breathing physiology, growth, and functional changes all further contribute to the high level of maxillary sinus differentiation.
The presence of a complex anatomical structure like the sinus is a critical factor influencing surgical treatment and implant rehabilitation of the posterior maxilla. The post-extraction remodeling and sinus pneumatization that often takes place after tooth loss can lead to alveolar bone atrophy necessitating grafting prior to implant placement.
When the atrophic bone is related to the pneumatization of the maxillary sinus, elevation of the sinus floor has been used to enable implant placement.22 Depending on the amount of residual bone, different bone-augmentation techniques have been proposed, including the lateral window approach described by Boyne and James (1980) and Tatum (1986).23, 24 The crestal approach, in which the Schneiderian membrane is lifted using an osteotome, was first described by Summers (1994).25 In both techniques, the simultaneous insertion of implants is recommended if the initial bone height is a minimum of 4 to 6 mm. 26 Otherwise a delayed insertion is preferred.27
While sinus augmentation has been demonstrated to be a predictable technique for increasing bone height in deficient posterior maxillary ridges prior to implant placement,28 the mean survival rates of implants placed in sinus-grafted areas are lower than those of implants placed in native bone after functional loading. 29, 30 Some recent studies have compared the survival rates of standard length implants (more than 8mm) in lifted sinus versus the use of short implants (≤8mm).31 These studies have clearly demonstrated comparable survival rates between longer implants in grafted sinus and extra short implants, but higher biological complications when a sinus lift was performed.32, 33 Sinus membrane perforation can occur more frequently in the augmented sinus than for extra short implants.31In order to reduce the complications, the surgical time, the costs and the morbidity the use of extra short implants can represent a valid surgical treatment if a correct and scrupulous cases selection is performed. 34
A valid alternative to prevent post-extraction alveolar bone atrophy and thus avoid the need for grafting can be immediate extraction placement. The immediate extraction placement technique, introduced in the 1970s,35 has become a common procedure for replacing hopeless teeth. Its major advantage is to reduce the duration and invasiveness of the treatment,36, 37, 38 yielding higher patient-satisfaction levels than delayed implant placement.39Immediate implant placement in the esthetic zone has become a therapeutic first choice for clinicians,40 while in molar regions, some difficulties must be overcome. The predictability of the post-extraction implant surgery in such sites depends upon the close approximation of the bone walls to the implant surface as well as the bone density, quality, and availability (Atieh et al. 2012).41, 42, 38 Some have argued that in order to achieve good primary stability at the time of immediate extraction placement, the bone apical to the root apex or the interradicular bone in case of multi-rooted teeth should be engaged by the implant threads.11, 12, 13, 14
The extension of the maxillary antrum and its relationship with premolar and molar roots can interfere with post-extraction implant placement. The available bone between the root apex and floor of the nose or sinus can only be precisely measured after a three-dimensional diagnostic examination. The present study demonstrates that in the first premolar area in about 25% of the cases there is little (< 3mm) or no bone apical to the root apex to engage with the implant. In the second premolar area, this percentage increases to almost 50%. Care should thus be taken when immediate extraction placement is performed in order to avoid sinus perforation during the preparation of the osteotomy.
The results of this study also indicate that interradicular sinus-floor invagination in the first molars occurs in about 50% of the cases, and in a lesser percentage in the second molars. More than 60% of the molars had an ISBH of less than 7mm. So immediate extraction placement of molars in the interradicular septum in most of the cases would require a small sinus elevation using a crestal approach (osteotome technique) for safe implant placement to minimize the risks of sinus-membrane perforation.
In all the CBCT scans that were analyzed, the distance between root apexes and maxillary sinuses was least for all the second premolars and first molars. This finding was not uniform, however, because of the anatomical variability of sinus growth.
One of the notable anatomical characteristics was the symmetry of the anatomical conditions in either side of each patient’s mouth. In the premolar and molar areas, the presence of root invagination inside the sinus was highly symmetrical both in terms of the presence or not of the invagination and in the amount of intrusion inside the antrum. This can probably be explained by the equivalent development of sinus pneumatization on both sides of the mouth and the fact that the premolar and molar roots on each side of any person’s mouth tend to be the same shape and length.
Conclusion
The data gathered in this study clearly show a close relationship between the maxillary root apexes and the inferior border of the sinus floor. Whenever CBCT or other radiological examination reveals the tooth apex to be in close proximity to the sinus floor, the use of short and wide diameter implants or a delayed approach should be considered preferable. Alternatively, if immediate extraction implant placement is being carried out, the use of osteotomes, rather than burs, to prepare an osteotomy that does not exceed the depth of the alveolus may minimize the risk of damaging the anatomical structures in the posterior maxilla.
References
- 1.Fugazzotto P A, Gulbransen H J, Wheeler S L, Lindsay J A. (1993) The use of IMZ osseointegrated implants in partially and completely edentulous patients: success and failure rates of 2.023 implant cylinders up to 60 months in function. Int J Oral Maxillofac Implants. 8, 617-621.
- 2.Leimola-Virtanen R, Peltola J, Oksala E, Helenius H, Happonen R P. (1995) ITI titanium plasma-sprayed screw implants in the treatment of edentulous mandibles: a follow-up study of 39 patients. , Int J Oral Maxillofac Implants; 10, 373-378.
- 3.Khatiblou F A. (2005) Sinus floor augmentation and simultaneous implant placement, part 1: the 1-stage approach. , J Oral Implantol2005;31(4);205-8
- 4.Misch C. (1993) Density of bone: effect on treatment planning, surgical approach and healing.In:Misch C,ed.Contemporary Implant Dentistry.St Louis,Mo:Mosby:. 469-485.
- 5.Wehrbein H, Diedrich P. (1992) Progressive pneumatization of the basal maxillary sinus after extraction and space closure [in German]. Fortschr Kieferorthop1992;. 53, 77-83.
- 6.Ohba T, Langlais R P, Morimoto Y, Tanaka T, Hashimoto K. (2001) Maxillary sinus floor in edentulous and dentate patients. , Indian J Dent Res2001; 12, 121-12.
- 7.Kopecka D, Simunek A, Brazda T, Rota M, Slezak R et al. (2012) Relationship between subsinus bone height and bone volume requirements for dental implants: A human radiographic study. , Int J Oral Maxillofac Implants2012Jan-Feb; 27(1), 48-54.
- 8.Ulm C W, Solar P, Gsellmann B, Matejka M, Watzek G. (1995) The edentulous maxillary alveolar process in the region of the maxillary sinus—A study of physical dimensions. , Int J Oral Maxillofac Surg 24, 279-282.
- 9.Jensen O T. (1999) Combined sinus grafting and Le Fort I Procedures. In:. Jensen OT (ed). The Sinus Bone Graft , Chicago: Quintessence 191-200.
- 10.Schleier P, Bierfreund G, Schultze-Mosgau S, Moldenhauer F, Küpper H et al. (2008) Simultaneous dental implant placement and endoscope-guided internal sinus floor elevation: 2-year post-load- ing outcomes. Clin Oral Implants Res. 19, 1163-1170.
- 11.Maksoud M A. (2001) Immediate implants in fresh posterior extraction sockets: report of two cases. , J Oral Implant 27, 123-126.
- 12.Crespi R, Capparè P, Gherlone E. (2010) Fresh socket implants in periapical infected sites in human.Journal PeriodontolMarch2010;81(3):. 378-383.
- 13.Bhale M, A L Neely, Kolhatkar S. (2008) Immediate implant placement:clinical decisions, advantages and disvantages.Oct2008;. 17(7), 576-581.
- 14.Penarrocha M, Uribe R, Balaguer J. (2004) immediate implants after extraction. A review of the current situation. , Med. Oral2004; 234-242.
- 16.Ulm C W, Solar P, Gsellmann B, Matejka M, Watzek G. (1995) The eden- tulous maxillary alveolar process in the region of the maxillary sinus—A study of physical dimensions. , Int J Oral Maxillofac Surg1995; 24, 279-282.
- 17.Hedesiu M, Balog C, Preda D M. (2008) The accuracy of alveolar crest dimensions measurement for dental implants. In vitro study. Rev Med Chir Soc Med Nat Iasi2008;. 112, 224-228.
- 18.Klinge B, Petersson A, Maly P. (1989) Location of the mandibular canal: Comparison of macroscopic findings, conventional radiography, and computed tomography. , Int J Oral Maxillofac Implants 4, 327-332.
- 19.Eberhardt J A, Torebinejad M, Christiansen E L. (1992) A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Surg Oral Med Oral Pathol.1992Mar;. 73(3), 345-6.
- 20.Sharan A, Madjar D. (2006) Correlation between maxillary sinus floor topography and related root position of posterio teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med oral Pathol Oral Endod.2006Sep:. 102(3), 375-81.
- 21.Yoshimine S, Nishihara K, Nozoe E, Yoshimine M, Nakamura N. (2012) Topographic analysis of maxillary premolars and molars and maxillary sinus cone beam computed tomography. Implant Dent.2012Dec;. 21(6), 528-35.
- 22.Jung Yun-hoa, Cho Bong-Hae. (2012) Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent.2012December;. 42, 219-224.
- 23.Tatum H Jr. (1986) Maxillary and sinus implant reconstruction. , Dent Clin North Am1986Apr; 30(2), 207-29.
- 24.Boyne P J, James R A. (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. , J Oral Surg1980Aug; 38(8), 613-6.
- 25.Summers R B. (1994) A new concept in maxillary implant surgery: the osteotome technique.Compendium1994Feb;158passim;quiz162,15(2);152,154-6.
- 26.Summers R B. (1994) The osteotome technique, part 3: less invasive methods of elevating the sinus floor.700,702–704passim.Compendium.1994;15:. 698.
- 27.Smiler D G, Johnson P, Lozada J. (1992) Sinus lift grafts and endosseous implants: treatment of the atrophic posterior maxilla. Dent Clin North Am. 36, 151-186.
- 28.Avila-Ortiz G, Wang H L, Galindo-Moreno P, Mish C E, Rudek I et al. (2012) Influence of lateral window dimensions on vital bone formation following maxillary sinus augmentation. Int J oral Maxillofac Implants. 27, 1240-1238.
- 29.Pjetursson B E, Tan W C, Zwahlen M, Lang N P. (2008) A systematic review of the success of sinus floor elevation and survival of implants in- serted in combination with sinus floor elevation. , J Clin Periodontol2008; 35, 216-240.
- 30.Wallace S S, Froum S J. (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol2003;. 8, 328-343.
- 31.Thoma D S, Zeltner M, Husler J, Hammerle C H, Jung R E. (2015) EAO Supplement Working Group 4- EAO CC 2015 Short implants wersus sinus lifting with longer implants to restore the posterior maxilla: a systematic review. Epub2015May21. Clin Oral Implants Res.2015Sep;26Suppl11: 154-69.
- 32.Felice P, Pistilli R, Piattelli M, Soardi E, Corvino V et al. (2012) Posterior atrophic jaws rehabilitated with prostheses supported by 5 x 5mm implants with novel nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Preliminary results from a randomized controlled trial.EurJOralImplantol2012Summer;5(2):. 149-61.
- 33.Guljè F L, Raghoebar G M, Vissink A, Meijer H J. (2014) Single crowns in the resorbed posterior maxilla supported by either 6-mm implants or by 11-mm implants combined with sinus floor elevation surgery: a 1-year randomised controlled trial.EurJOralImplantol2014Autemn;. 7(3), 247-55.
- 34.Lemos C A, Ferro-Alves M L, Okamoto R, Mendonça M R, Pellizzer E P. (2016) Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis.JDenta.2016Apr;Epub2016Jan19,47:. 8-17.
- 35.Shulte W, Kleineikenscheidt H, Lindner K, Schareyka R. (1978) The Tubingen immediate implant in clinical studies (in German). Dtsch Zahnarztl Z. 33, 348-359.
- 36.Barzilay I, Graser G N, Caton J, Shenkle G. (1988) I mmediate implantation of pure titanium threaded implants into extraction sockets. , J Dent Res1988; 67, 234.
- 37.Barzilay I, Graser G, Iranpour B, Natiella J R. (1991) Immediate implantation of a pure ti- tanium implant into an extraction socket: Report of a pilot procedure. Int J Oral Maxillofac Implants. 6, 277-284.
- 38.Lazzara R J. (1989) Immediate implant placement into extraction sites: Surgical and restorative advantages. , Int J Periodontics RestorativeDent 9, 332-343.
- 39.Quirynen M, N Van Assche, Botticelli D, Berglundh T. (2007) How does the timing of implant placement to extraction affect outcome? Int J Oral Maxillofac Implants. 22, 203-23.
- 40.Atieh M A, Ahmad A H, AGT Payne, Duncan W J. (2009) Immediate loading with single implant crowns: A systematic review and meta-analysis. , Int J Prosthodont2009; 22, 151-160.
Cited by (2)
- 1.Morsy EsraaK, El Dessouky SaharH, Abdel Ghafar EnasA, 2022, Assessment of proximity of the maxillary premolars roots to the maxillary sinus floor in a sample of Egyptian population using CBCT: An observational cross-sectional study, Journal of International Oral Health, 14(3), 306, 10.4103/jioh.jioh_355_21
- 2.Milenkovic Jovana, Vasiljevic Milica, Jovicic Nemanja, Milovanovic Dragan, Selakovic Dragica, et al, 2022, Criteria for the Classification of the Interradicular Septum Shape in Maxillary Molars with Clinical Importance for Prosthetic-Driven Immediate Implant Placement, Diagnostics, 12(6), 1432, 10.3390/diagnostics12061432
