Abstract
Background/Aims:
Thyroid disorders are a common, worldwide clinical problem in general practice.It presents predominantly as a thyroid nodule. Each thyroid nodule has a risk of cancer. The incidence of thyroid cancer is much more common in Saudi Arabia in comparison to the West. There is a worldwide increase in the incidence of thyroid cancer. The objective of this study is to highlight in details the wide spectrum of histopathologic diagnosis encountered in patient undergoing thyroid surgery in the population of Riyadh region of Saudi Arabia.
Patients and Methods:
Retrospective review of all thyroid samples for 256 patients whom underwent thyroid surgery at King Khalid University Hospital, King Saud University, Riyadh, during the period between 2000 and 2009. Of those, 171 cases were non neoplastic and 85 neoplastic lesions. Females constitute 80% of non neoplastic lesions and 79% of all thyroid malignancies. The peak incidence of thyroid cancer was in the third decade. Papillary thyroid carcinoma was the most common cancer (71%).
Conclusion:
Thyroid cancer is a common cancer in Saudi Arabia; it is the second most common cancer in females. The increasing rates of thyroid cancer occur predominantly in women. Papillary thyroid carcinoma accounted for the bulk of this increase. Additional studies are needed to explain the rise in papillary thyroid carcinoma incidence in Saudi Arab as well as throughout the world and to search potential risk factors that are currently unrecognized.
Author Contributions
Academic Editor: Erxi Wu, Department of Pharmaceutical Sciences, North Dakota State University, US
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Emad Raddaoui, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction:
After diabetes mellitus, among the endocrine organs disorders, thyroid lesions are quite commonly encountered in the clinical practice. Thyroid nodules are very common and of concern (because of the risk of malignancy and hyperfunction) occurring in 3% of the population, more commonly in females and in areas of iodine deficiencies. Almost one third of the world’s population lives in the areas of iodine deficieny1. There is a well known geographical dependency in thyroid disease because of the different amount of alimentary iodine intake that occurs in different geographical locations2. The form of thyroid disorders includes non toxic goiter, Grave’s disease, Hashimotos thyroiditis and thyroid neoplasms.
Thyroid neoplasms account for only 1% of the overall human cancer burden, however they represent the most common malignancies of the endocrine systems (90% of all endocrine cancers).They are responsible for more deaths than any other endocrine cancers3. According to 2012 United States cancer statistics reporting, thyroid cancer is expected to be the 5th most commonly diagnosed cancer among women. The incidence of thyroid cancer is much more common in Saudi Arabia (SA) as compared to the western world. It is the second most common malignancy after breast cancer in female patients4. The reasons for this increase remain unclear and controversial. Several studies suggest that the rise is likely related to greater diagnostic scrutiny and subclinical detection. The basis for these claims are supported by studies demonstrating a concomitant rise in the use of imaging modalities of the neck and detailed histologic evaluations of thyroidectomy surgical specimens that have increased concomitantly with the rise in thyroid cancer diagnoses5, 6. Hence they pose a significant challenge to the pathologist, surgeon and oncologists. Thyroid cancer occurs primarily in young and middle aged adults with approximately 122000 new cases per year world wide according to the world cancer report, IRRC7.
In SA, according to the 2011 King Faisal specialist Hospital and research center (KFSH&RC ) analytics report, 9.5% of all malignancies in KFSH&RC are thyroid cancer, much higher than in the West. It represents 12.6% of female malignant neoplasms, second to breast cancer. The male/female ratio is 0.3:1. Thyroid cancer accounts for only 3% of all cases in the U.S.A., and 4.7% of female malignancies.
The main goal of present study was to expand on the previous reports; the pattern of surgically treated thyroid diseases and to describe the epidemiology and the spectrum of histological diagnosis encountered in patients undergoing thyroid surgeries in the population of Riyadh region of SA in more detail.
Materials and Methods
A retrospective review was conducted of all the patients who underwent thyroid surgery between 2000 and 2009 at King Khalid University hospital, King Saud University in the Riyadh, SA.
All patients presenting with thyroid swelling and undergoing any type of thyroid operation were included in the study. Those patients in whom fine needle aspiration cytology (FNAC) was done but they did not undergo thyroid surgery were excluded from the study. FNAC was carried out in patients having dominant or solitary nodule. All the surgically excised thyroid specimens were 10% buffered formalin fixed and paraffin embedded. The sections were stained using Haematoxylin and Eosin stains (H&E). The reports, slides and blocks were kept in the department archives. All sections were diagnosed and reported by pathologists. Detailed information including name, age, gender, tumor site and histology were recorded. Several prognostic factors were stratified and sub stratified by age and gender.
Thyroid cancers were histopathologically distributed as papillary carcinoma, follicular carcinoma, poorly differentiated carcinoma, anaplastic carcinoma, hurthle cell carcinoma, dedifferentiated thyroid carcinoma and medullary carcinoma. Papillary thyroid carcinoma were further sub classified as classical papillary carcinoma, encapsulated variant of papillary carcinoma, microscopic papillary thyroid carcinoma and follicular variant of papillary carcinoma.
All PTC cases showing presence of distant metastasis to organs like lung, liver, bone, etc. were classified as M1 (American Joint Committee on Cancer definition). Extra thyroidal extension was defined as extension of the tumor outside the capsule as documented in the histopathology reports. The data analysis was carried out using the SPSS statistical software package.
Results:
Total number of thyroidectomies performed in our institution over a nine years period was 256, of which 171 cases were non neoplastic, 85 neoplastic; of those 23 cases were adenomas and 62 cases were malignant (Table 1). The non neoplastic lesions (multi nodular goiter and auto immune thyroiditis) peak frequency was in third to fifth decades (Table 2). The youngest patient in our series was twelve years male with colloid nodule. The age ranged from 12 years to 78 years. Of the total non neoplastic lesions, there were 142 females constituting 80% in this series and the male to female ratio was 4:1. Female accounted for 99 cases (80%) of the multi nodular goiter, 14 cases (93%) of goiter and thyroiditis, 20 cases (95.2%) of Hashimoto’s thyroiditis (Figure 1) and 8 cases (80%) of colloid nodule.
Table 1. Distribution of various thyroid pathology in different age group| Age Group | Benign cases(n=171) | Solitary adenomas(n=23) | Thyroid cancer(n=62) |
| <20 | 5 | 1 | 2 |
| 20-29 | 19 | 3 | 9 |
| 30-39 | 49 | 4 | 22 |
| 40-49 | 43 | 7 | 16 |
| 50-59 | 37 | 7 | 10 |
| 60-69 | 12 | 1 | 2 |
| 70-79 | 6 | 0 | 1 |
| Diagnosis Age range | Less than 20 years | (20-29)years | (30-39)years | (40-49)years | (50-59)years | (60-69)years | (70-79)years | |||||||
| Thyroid carcinoma | M | F | M | F | M | F | M | F | M | F | M | F | M | F |
| 1 | 1 | 3 | 6 | 2 | 20 | 3 | 13 | 4 | 6 | 0 | 2 | 0 | 1 | |
| Follicular adenoma | 1 | 0 | 1 | 2 | 0 | 3 | 2 | 3 | 1 | 3 | 0 | 1 | 0 | 0 |
| Hurthle cell adenoma | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 3 | 0 | 0 | 0 | 0 | 0 |
| MNG | 1 | 2 | 1 | 6 | 7 | 26 | 4 | 29 | 7 | 23 | 2 | 9 | 2 | 4 |
| Goiter +thyroiditis | 0 | 0 | 1 | 1 | 0 | 6 | 0 | 4 | 0 | 2 | 0 | 0 | 0 | 0 |
| Colloid nodule | 1 | 0 | 0 | 4 | 0 | 1 | 0 | 3 | 0 | 0 | 1 | 0 | 0 | 0 |
| Hashimotos | 1 | 0 | 0 | 3 | 0 | 9 | 0 | 3 | 0 | 5 | 0 | 0 | 0 | 0 |
| Graves ds | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Figure 1.High power view showing Hashimoto’s thyroiditis with lymphocytic infiltrate in the periphery and Hurthle cells {asterisk} in the center. (Hematoxylin & eosin, original magnification ×400).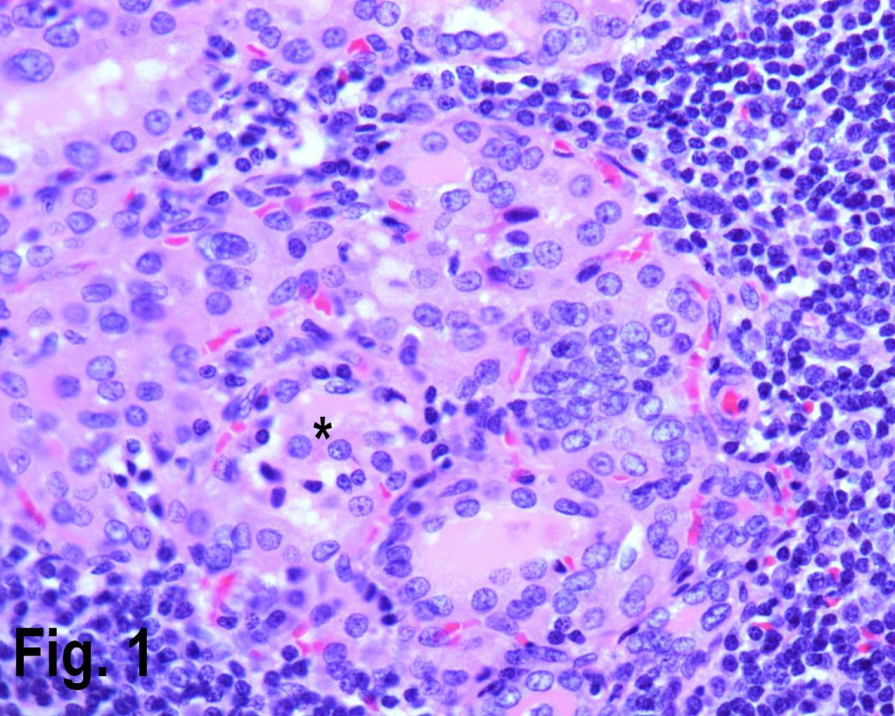
Solitary benign adenomas were found in 23 cases, the peak frequency was fourth and fifth decade. Female accounted for 12 cases (70.5%) for follicular adenoma (Figure 2) and 3 cases (50%) for Hurthle cell adenoma. Thyroid malignancy and it was reported in 62 cases. Papillary carcinoma (Figure 3) was the most common type of thyroid malignancy found in 44 cases (71%) followed by follicular carcinoma (9.6%) (Figure 4), medullary carcinoma (1.6) and poorly differentiated carcinoma (1.6%) (Table 3). The peak incidence for patients with thyroid malignancy in this series was third decade and male to female ratio was 3.7:1.
Figure 2.Low power view showing a follicular adenoma. (Hematoxylin & eosin, original magnification ×200).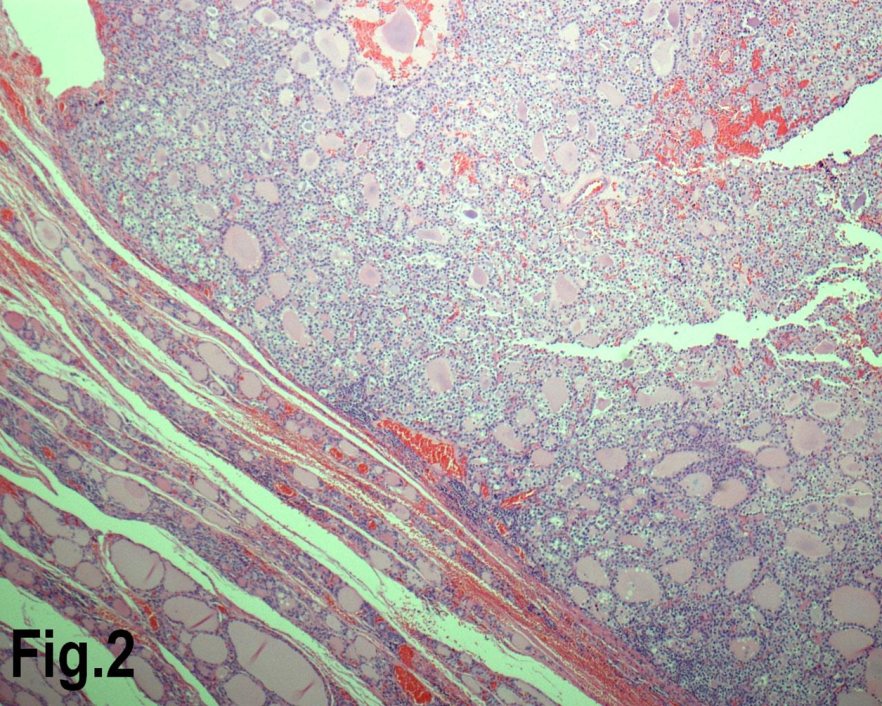
Figure 3.High power view showing follicles lined by cells with nuclear characteristics of papillary carcinoma, with prominent intra nuclear inclusions (Hematoxylin & eosin, original magnification ×400).
Figure 4.Low power view showing a follicular carcinoma with capsular invasion. (Hematoxylin & eosin, original magnification ×200).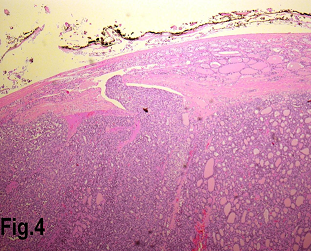
| Pathology | TOTAL | Females | Males | |||
| n | % | n | % | n | % | |
| Papillary Carcinoma(Classical) | 20 | 32.2 | 16 | 32.6 | 4 | 30.7 |
| Papillary Carcinoma(Microscopic) | 10 | 16.1 | 9 | 18.3 | 1 | 7.7 |
| Papillary Carcinoma](Encapsulated) | 5 | 8.06 | 3 | 6.1 | 2 | 15.3 |
| Papillary Carcinoma(Follicular variant) | 19 | 30.6 | 14 | 28.5 | 5 | 38.4 |
| Follicular carcinoma | 6 | 9.6 | 5 | 10.2 | 1 | 7.7 |
| Medullary Carcinoma | 1 | 1.6 | 1 | 2.0 | 0 | 00 |
| Poorly differentiated carcinoma | 1 | 1.6 | 1 | 2.0 | 0 | 00 |
| TOTAL | 62 | 100 | 49 | 100 | 13 | 100 |
Discussion:
Thyroid disorders are one of the common problems encountered in clinical practice with majority of them benign in nature. Today thyroidectomy is a routine procedure because of the introduction of safe anesthesia, antiseptics, fine surgical instruments and developments of new techniques, offering the chances of cure to many patients8, 9.
In this study, multi nodular goiter contributed 122 cases (47.6%) forming the most common presenting pathologic presentation. A high incidence of multi nodular goiter was also reported in Bisha10, Jeddah11 and Asir12 region of SA and Pakistan13. However in a study published from Nigeria9 reported colloid goiter to be the most common type of benign pathology in thyroid.
Females (80%) preponderance of benign thyroid disease was observed in this study over males (20%) making male female ratio of 4:1, this was in agreement with studies done in other areas. The thyroid disease particularly multi nodular goiter was seen in almost all age group (30-59 years) which was similar to other observations9, 10, 11, 12, 13.
In SA, thyroid cancer is the second most common malignancy after breast cancer in female patients14. Differentiated thyroid carcinoma in SA accounted for 3.9-5% of all cancers and was observed as the most frequent endocrine malignancy. This figure was reported in 3 earlier series from Riyadh and Jeddah, SA15, 16, 17. According to tumor registry annual report 2011 published from KFSH&RC, Riyadh; SA 18, 9.5% of all malignancies in KFSH&RC are thyroid cancers, much higher than in the West.
It represents 12.6% of female malignant neoplasms, second to breast cancer. The male/female ratio is 0.3:1. Thyroid cancer accounts for only 3% of all cases in the U.S.A., and 4.7% of female malignancies.
In present study, we found that the increasing rates of thyroid cancer occur predominantly in women. Differentiated thyroid carcinoma accounted for the bulk of this increase and accounted for 61 out of total of 256 cases (23.8%). This figure is higher than previously reported in Abha, SA19 and found in the republic of Yemen20.
Majority of our thyroid cancer patients present in 30-59 years age group. However, the age distribution is more widely distributed with majority presenting at a younger age in 3rd and 6th decades of life. According to the study performed in Spain21, Scotland22 papillary thyroid carcinoma was the predominant type (76%) with increase in both the micro papillary and in papillary thyroid carcinoma measuring more than 1 cm in size.
Follicular carcinoma contributed 2.34% (6 cases out of 256) indicating lower incidence of this type of malignancy in our area. This is in contrast to incidence in Africa23 and Nigeria9.
The incidence of medullary carcinoma is less than 1% in most of the studies mentioned above. Also no anaplastic, hurthle cell carcinoma or lymphoma was found in our study. This is similar to the study performed in Bisha19 and Medinah24 area of SA, where no such cases were identified in their study.
There are several possible explanations as to why thyroid cancer is significantly more frequent in SA as compares to other countries in the world. These include female sex, having a history of goiter or thyroid nodules, a family history of thyroid cancer, and radiation exposure related to medical treatment during childhood. Radiation exposure as a result of radioactive fallout from atomic weapons testing and nuclear power plant accidents has also been linked to increased risk of thyroid cancer, especially in children. Certain rare genetic syndromes also increase risk. People who test positive for an abnormal gene that causes a hereditary form of thyroid cancer can decrease the chance of developing the disease by surgical removal of the thyroid gland. Unlike other adult cancers, for which older age increases risk, 80% of newly diagnosed thyroid cancer patients are under 65 years of age14.
Thyroid cancer incidence is increasing throughout the world. Most studies attribute this rise entirely to the increase in papillary thyroid carcinoma incidence, the most common thyroid malignancy in iodine sufficient areas. Some researchers suggest that this rise is only apparent due to an increase in diagnostic activity.
Conclusion:
In SA, in past several decades, there is relative increase in the incidence of both non neoplastic and neoplastic disorders. This data should be taken into account when planning the health resources for these patients. Additional studies are needed to explain the rise in papillary thyroid carcinoma incidence in SA as well as throughout the world and to search potential risk factors that are currently unrecognized.
References
- 1.Mackenzie E J, Mortimer R H.6: Thyroid nodules and thyroid cancer. , Med J Aust.2004Mar 180(5), 242-7.
- 3.Knudsen N, Bülow I, Jørgensen T, Laurberg P, Ovesen L et al. (2000) Comparative study of thyroid function and types of thyroid dysfunction in two areas in Denmark with slightly different iodine status. , Eur J Endocrinol.2000Oct; 143(4), 485-91.
- 4.Boone R T, Fan C Y, Hanna E Y.Well-differentiated carcinoma of the thyroid. , Otolaryngol Clin North Am.2003Feb; 36(1), 73-90.
- 5.Bazarbashi S. (2004) Saudi Cancer Registry. Cancer Incidence Report. Riyahd (KSA): Saudi Cancer Registry;2008.p. 1-98.
- 6.Grodski S, Brown T, Sidhu S, Gill A, Robinson B et al. (2008) Increasing incidence of thyroid cancer is due to increased pathologic detection. , Surgery.2008Dec; 144(6), 1038-43.
- 7.Hall S F, Walker H, Siemens R, Schneeberg A.Increasing detection and increasing incidence in thyroid cancer. , World J Surg.2009Dec; 33(12), 2567-71.
- 9.Burguera B, Gharib H.Thyroid incidentalomas. Prevalence, diagnosis, significance, and management. , Endocrinol Metab Clin North Am.2000Mar; 29(1), 187-203.
- 10.Nggada H A, Ojo O S, Adelusola K O.A histopathological analysis of thyroid diseases in Ile-ife, Nigeria. a review of 274 cases. , Niger Postgrad Med J.2008Mar; 15(1), 47-51.
- 11.Al Ghamdi SA, Raza M A, Hanif S, Al Shehri G.The pattern of surgically treated thyroid diseases in the Bisha Region of Saudi Arabia. Ann Saudi Med.2002Sep-Nov; 22(5-6). 410-412.
- 12.Nasr H A.Surgically treated goiter at King Abdulaziz University Hospital. Jeddah, Saudi Arabia.8 Saudi Medical Conference,1983(Abstracts). King Khalid Academy,Riyadh,1983,78 .
- 13.Abu-Eshy S A, Abolfotouh M A, Al-Naggar Y M.Endemic goitre in schoolchildren in high and low altitude areas of Asir region, Saudi Arabia. Saudi Med J.2001Feb;. 22(2), 146-9.
- 14.Nazar H, Anwar M, Nadia N, Zulfiqar A.Pattern of surgically treated thyroid disease. in KARACHI. Biomedica. 2005.Jan. – Jun;21 .
- 15.Hussain F, Iqbal S, Mehmood A, Bazarbashi S, ElHassan T et al.Incidence of thyroid cancer. in the Kingdom of Saudi Arabia, 2000-2010. Hematol Oncol Stem Cell Ther.2013Jun; 6(2), 58-64.
- 16.Al-Salamah S M, Khalid K, Bismar H A.Incidence of differentiated cancer in nodular goiter. Saudi Med J.2002Aug; 23(8), 947-52.
- 17.Ahmed M, Al-Saihati B, Greer W, Al-Nuaim A, Bakheet S et al.A study of 875 cases of thyroid cancer observed over a fifteen-year period (1975-1989) at the King Faisal Specialist Hospital and Research Centre. Ann Saudi Med.1995Nov;. 15(6), 579-84.
- 18.Al-Balawi I A, Meir H M, Yousef M K, Nayel H A.Al-Mobarak MF. Differentiated thyroid carcinoma referred for radioiodine therapy. Saudi Med J.2001Jun;. 22(6), 497-503.
- 19. (2011) King Faisal Specialist Hospital Tumor Registry Annual Report. Available from http:// www.kfshrc.edu.sa/oncology/Tumor
- 20.Refeidi A A, Al-Shehri G Y, Al-Ahmary A M, Tahtouh M I, Alsareii S A.. Al-Ghamdi AG,Mahfouz AA, Abu-Eshy SA. Patterns of thyroid cancer in Southwestern Saudi Arabia. Saudi Med J.2010Nov; 31(11), 1238-41.
- 21.Al-Jaradi M, Sallam A, Jabr H, Borda A, Decaussin-Petrucci M et al.Prevalence of differentiated thyroid cancer in 810 cases of surgically treated goiter in Yemen. Ann Saudi Med.2005Sep-Oct;. 25(5), 394-7.
- 22.Rego-Iraeta A, Pérez-Méndez L F, Mantinan B, Garcia-Mayor R V.Time trends for thyroid cancer in northwestern Spain: true rise in the incidence of micro and larger forms of papillary thyroid carcinoma. , Thyroid.2009Apr; 19(4), 333-40.
- 23.Reynolds R M, Weir J, Stockton D L, Brewster D H, Sandeep T C et al.Changing trends in incidence and mortality of thyroid cancer in Scotland. Clin Endocrinol (Oxf).2005Feb;. 62(2), 156-62.
