The Role and Effect of the Comprehensive Music Therapy in Project Sleep: A Multi-Disciplinary Quality Improvement Project.
Abstract
Sleep is vital for the maintenance of physical health and mental wellbeing. Sleep also plays a cardinal role in the process of healing. It is estimated that 50 to 70 million Americans suffer chronically from sleep disturbances and insufficiency, which not only hinders daily functioning but also adversely affects health, quality of life and longevity.1 Deficient sleep is associated with an increased risk of developing chronic diseases such as hypertension, diabetes, obesity, heart disease, stroke, depression, frequent mental distress, as well as increased mortality, and reduced quality of life and productivity.1,2Aging, medical conditions, pain, and mental illness further aggravate sleep disturbances such as insomnia, sleep fragmentation and daytime sleepiness.3, 4, 5, 6, 7, 8
The a common treatment for sleep disturbances and insomnia is pharmacological therapy. Benzodiazepines may have negative long-term side effects including residual daytime sedation and tolerance development. Withdrawal difficulties may increase dependency. In the older patient there are safety issues related to daytime sedation including increase risk of falls. With the importance of sleep in hospital recovery and the side effects of sleep medication becoming more widely recognized, there has been an impetus to s use nonpharmacological alternatives , such as music.. This pilot study builds on the potential impact of music’s effectivity by introducing music therapy as a safe, cost effective and culturally sensitive intervention.
Author Contributions
Academic Editor: He Jinbo, University of Macau, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Chang-LitW.et al
 This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Sleep is vital for the maintenance of physical health and mental wellbeing. Sleep also plays a cardinal role in the process of healing. It is estimated that 50 to 70 million Americans suffer chronically from sleep disturbances and insufficiency, which not only hinders daily functioning but also adversely affects health, quality of life and longevity.1 Deficient sleep is associated with an increased risk of developing chronic diseases such as hypertension, diabetes, obesity, heart disease, stroke, depression, frequent mental distress, as well as increased mortality, and reduced quality of life and productivity.1,2 Aging, medical conditions, pain, and mental illness further aggravate sleep disturbances such as insomnia, sleep fragmentation and daytime sleepiness.3, 4, 5, 6, 7, 8
Patients in acute care hospitals are more likely to be geriatric with multiple comorbidities. This population is more likely to have issues related to insomnia and poor sleep.22,23,24Medical nighttime routines can disrupt sleep and the active environment of the hospital can exacerbate insomnia. Sleep can affect pain, anxiety, mood, cognitive function and immune system.1,2,3,4,7,8,25,26 Pharmacologic agents used for sleep can lead to delirium, increased falls rate, prolonged hospitalization and a decrease in patient satisfaction.27,28,29
A common treatment for sleep disturbances and insomnia is pharmacological therapy. Benzodiazepines may have negative long-term side effects including residual daytime sedation and tolerance development. Withdrawal difficulties may increase dependency.
Among older patients, there are safety issues related to daytime sedation including increased risk of falls. With the importance of sleep in hospital recovery and the side effects of sleep medication becoming more widely recognized, there has been an impetus to use nonpharmacological alternatives, such as music.
This article will focus on the music therapy element of Project Sleep: a multidisciplinary quality improvement project utilizing non-pharmacological methods to improve quality of sleep for patients during hospitalization. In this pilot study, we will examine the potential impact and effectivity of music in enhancing quality of sleep by introducing music therapy as a safe, cost effective and culturally sensitive intervention. Although it is important to note that the result presented in this article was not yielded solely by music therapy, the comprehensive music therapy program, developed by the Louis Armstrong Center for Music and Medicine, is an innovative and unique approach that recognizes and utilizes the versatility of music to address the complexity of sleep disturbance during hospitalization. Description and implementation of the music therapy interventions within the group, individual, community and procedure setting context provided through Project Sleep reflect aspects of how sleep may be induced and/or enhanced when provided by a multidisciplinary team alongside an integrative medical team and environment.
Project Sleep
Project Sleep was a multidisciplinary endeavor designed to use cost effective and non- pharmacological methods to enhance inpatient quality of sleep with the goals of reducing the use of zolpidem, improving patient experiences and decreasing falls.27Interventions from HELP study ((Hospital Elder Life Program) and a sleep pilot at Mount Sinai Roosevelt Hospital27,28,29,30,31,32,33 were used as a starting point to develop an inpatient sleep intervention at Mount Sinai Beth Israel. The study was piloted on a medical unit that had a history of low patient satisfaction scores resulting from what was reported on surveys as a high volume noise level with the most amount of 4-bedded rooms. The patient population is diverse, with a mixture of geriatric patients, palliative patients, as well as adult patients with psychiatric comorbidities and/or substance abuse.
Recognizing the impact of music therapy and its capacity and potential to ameliorate noxious sound environments on ICUs within the hospital36 as well as improving quality of sleep, the Louis Armstrong Center for Music Medicine team participated in the design of the project to enhance the program with music therapy.
Methods
The multidisciplinary core team includes Geriatricians, Hospitalists, Nurses, Pharmacists, Music Therapists, and Housestaff. We designated a pilot inpatient medical unit for the project and administered a 5-question sleep survey to 125 patients (Appendix II), which served as our pre-intervention group over a period of 10 months.
The Project Sleep protocol included:
Instituting quiet hours (10PM to 6AM) during which time vital sign checks & blood draws were minimized.
Educational material and posters promoting healthy sleep habits to patients, visitors and medical staff.
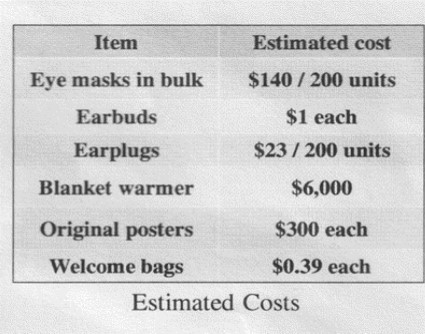
Sleep promotion “welcome bags” were distributed upon patient admission. The bags contain an explanation of the project, headphones, an eye mask, and earplugs.
Offerings of with warm blankets, warm milk & tea for night time comfort.
Melatonin was introduced as an alternative to sedative-hypnotics.
Acupuncture is offered upon request.
Comprehensive music therapy service is provided and a multicultural lullaby channel is produced and programmed on each patient TV for easy accessibility to music during evening hours.
Upon implementing these changes, project sleep team administered the same 5-question sleep survey to 125 different patients, and this served as our post-intervention group. We also performed ongoing analysis of the unit’s HCAHPS scores, zolpidem prescribing patterns & falls.27
Comprehensive Music Therapy Interventions
Recognizing the potentially detrimental impact of noise on perceived stress among patients, family members, and medical staff, the LACMM not only offered individual music therapy to patients, but at the same time provided Environmental Music Therapy (EMT)34,35,36for the patient and staff common areas. We sought to mitigate the, at times, harsh auditory environment on the unit. In addition, a Caring for Caregivers music group afforded the opportunity for medical staff to de-stress and restore energy; and Music Therapy Groups designed for patients and their family members facilitated tension-release opportunities and forums for potential socialization. Within comprehensive music therapy protocol, we also developed and produced a multicultural lullaby album as a CD. It was also programmed onto each patient TV, addressing the requests for evening music and highlighted the rich cultural diverse patient populations represented at Mount Sinai Beth Israel Medical Center in downtown New York City.
Table 1. Comprehensive Music Therapy| Comprehensive Music Therapy Interventions | Caring for | Music Therapy | Individualized | Multicultural |
| Caregiver | Group | Medical Music | Lullaby CD on Patient | |
| Psychotherapy | TVs | |||
| 20min x2/week | 30min x2/week | Mon-Fri upon referral |
Environmental Music Therapy (EMT)
Although sleep is essential for healing and wellness, the hospital environment- a place that is meant to be conducive to healing- in reality can be disruptive to a patient’s healthy sleep cycle. There have been bodies of literature in medical journals illuminating how hospital noises,37,38,39,40 inclusive of beeping of medical equipment, intercoms, phones ringing, TV noise and people speaking, not only can precipitate and exacerbate stress and anxiety but also can influence the perception of pain and quality of care. Noise exposure can contribute to a number of short-term physiological responses mediated through the autonomic nervous system. High volume, erratic, and noises in higher (machine beeping) or lower (AC roaming) frequencies can cause physiological activation of ‘fight or flight’ response- including elevated heart rate, respiratory rate and blood pressure, peripheral vasoconstriction and higher levels of adrenaline and cortisol- or the stress hormones.39,40,41,42 Although such a physiological response is designed to ensure survival, encouraging a potential escape from actual danger, our bodies can work against us when the hospital environment is perceived as hostile. The prolonged recurrence of a stress response caused by environmental noise can directly impact sleep, increase anxiety, anger, or feelings of annoyance and depressiveness;43,44,45,46.it also can suppress the immune system. 47,48,49,50. Poor sleep health can exacerbate the physiological, psychological and psychosocial condition of patients, particularly those with neurologic dysfunction. Compounded problems of heightened stress and disturbed sleep can delay recovery, thus prolonging hospitalization.36,37,38,46,47,48,49
The music therapy component of Project Sleep was implemented as a strategic means of addressing the noise. The LAMM’s EMT program was provided twice a week for 45 minutes in the early- afternoon, which was identified by the nursing manager as often the busiest and the most stressful time in the day. Certified music therapists addressed patient and caregiver stress within the environment utilizing a group-assessment strategy. Through integrating the sounds, moods, rhythm and shared expressions directly within the environment as musical elements, music therapists create a holding space, providing a sense of structure and organization, which would soften the environmental noise. EMT begins with improvisation, which allows the therapists to flexibly incorporate the sound elements into the music.34The music gradually transitions to familiar melodies (instrumental or song) reflective of the culture, age groups, and ethnicities through request and extension of requested eras, and through desired arrangement based on the patient and staff recipients’ movement, discussion, activity level. Music therapists facilitate EMT according to moment-by-moment observation and interaction with individuals in the space, creating a “soundtrack” of the ambience.34,35,36 With sensitivity and intention in administering the music, music therapists gradually transform the sound environment into a calmer-or more uplifting- and safer atmosphere as the intrusive and chaotic noise melds and seemingly evaporates into the music.34,35,36,35,34,33,32,31 The sense of safety is essential in increasing feelings of comfort, reducing stress level, promoting quiet social interaction, inducing relaxation, which all potentially render improved quality of sleep.
Caring for the Caregiver
Self-care in helping professions is essential to ensure best quality of patient care and career longevity.52 However, in a busy and high-pressure medical environment, it is often neglected. Literature within the past two decades has raised the awareness of the susceptibility to compassion fatigue and/or burnout amongst healthcare professionals as well as recognizing the need to develop ways to care for the caregivers.52,53,54,55,56 Compassion fatigue- also called vicarious traumatization or secondary traumatization57- is the emotional residue or strain of exposure to working with those suffering from the consequences of traumatic events. It differs from burn-out, but can co-exist. Researchers have recognized that healthcare professionals may experience trauma symptoms similar to those of their clients.57,58 When health care professionals struggle with their responses to the trauma suffered by their patients, they are at risk of compromising their own mental and physical health, relationships, and effectiveness at the workplace.56,57,58 Symptoms of compassion fatigue may range from psychological issues such as dissociation, anger, anxiety, sleep disturbances, nightmares, feeling powerless, to physical symptoms such as nausea, headaches, general constriction, dizziness, and impaired hearing.56,57,58,58 The negligence of self-care and a lack of built–in systematic support to counter compassion fatigue in the medical environment, can result in higher rates of burnout, depressive symptoms, and may increase suicide risk among physicians, medical residents, nurses and social workers.52,55,56,57,58,59,60
Music therapy literature has long recognized the effectiveness of music in providing a venue and containment to safely express and process loss, grief and trauma. But it was the catastrophe on 9/11/2001 that shed the light on the magnitude of the impact of trauma and the importance in caring for the caregivers. New York based music therapists organized initiatives soon after the disaster through American Music Therapy Association NYC Music Therapy Relief Project and the Caring for the Caregiver Program, providing more than 7000 music therapy interventions over six months to children, adults, caregivers, and families affected by the attacks on the Twin Towers.61 Dr. Joanne V. Loewy, the director of the Armstrong Music therapy program at Mount Sinai Beth Israel Medical Center, developed the Caring for the Caregiver program, expanding the concept of “caregiver” to “those who could benefit from experiencing, understanding, expressing, and educating themselves about trauma through music”(p.1)61with the realization that it was difficult to separate personal loss from and the loss experienced through professional encounter with a disaster in such magnitude. According to the project coordinator, Kirsten Stewart, the program was a 9-week series of trainings, each 90 minutes in length divided into two segments; “One containing an experience of using music as a means of cope, and the other containing emotional and educational perspectives on how to move through the effects of anger, silence, depression, and fear associated with coping from the experience of traumatic events”. (p. 15)61 Through interventions such as improvisation, song-writing and singing, stories, discussions, listening, relaxation, drawings, reading, imagery, and bodywork, caregivers were able to find a way to retrieve the wealth of inner resources and strength for themselves and other.61,62
As part of the multi-disciplinary collaboration of Project Sleep, the LACMM places significance in enhancing the emotional well-being of our medical staff, which directly influences the quality of patient care/customer service. We provided Caring for Caregiver61music therapy groups to team of medical staff twice a week. This particular intervention was challenging to administer initially as the medical staff often expressed that they were “too busy” to take time for themselves. To address the dilemma, the therapist worked together with the nurse manager, who would remind and encourage his staff members to utilize the service. With the critical ‘blessing’ from the nurse manager, the staff members became more proactive in taking time for participating music-assisted meditation, singing their favorite songs, and/or playing percussive instruments to release both physical and emotional tension. Our caring for caregiver groups took place initially in the patient lounge. Being permitted to leave their posts for even just a couple of minutes- both physically and metaphorically- the staff were able to focus the care on themselves, to optimally release their tension and stress through active music making. They were able to achieve a deeper relaxing state through music-assisted visualization with deep breathing techniques in a contained and safe space. Caring for Caregiver groups have taken many forms to address the needs of the staff members. They also address the ever-changing circumstances of the unit.
One significant example demonstrates the importance and direct benefits of our ‘caring for caregiver’ music therapy.61
It was a steamy day in July and the atmosphere on the unit was heavy. The attending physician pulled me aside and expressed that it was a difficult day for her and her staff because a patient had died unexpectedly. Recognizing the need for emotional support, I invited the physician and her staff to take a moment to come to the patient lounge. I held the space with the guitar, ocean drum and voice as staff trickled in and sat down. I improvised gently, entraining to the collected rhythm and energy in the room. I used finger picking on the guitar, providing harmonic tension and release with dissonant intervals resolving into consonant ones. Sustained and descending vocal lines were implemented to create a linear motion that not only encouraged deeper breath but also provided a sense of direction for visualization. Many sighed as they tried to breathe. I continued to hold the emotional space with gentle improvised music in ¾ meter to provide a rocking pulse to elicit feelings of safety while including harmonic tension release to meet their emotional state. I then guided their awareness to their breath and bodies. Some staff members began to actively release their tension. Most of the members’ breathing became deeper and slower with the music. I continued to guide the experience and suggested for them to visualize a “safe place”. This was to encourage a retrieval of their inner resources. The music was held in ¾ meter with the voice and the harmonic cushion created by the guitar in Mixolydian mode, combining with the imagery of a safe place, further elicited physiological relaxation responses that allowed the staff members to feel centered and grounded. The group was attended by two nurses and two nursing assistants, along with the physician, who later joined the experience. As the staff members’ breathing gradually became deeper and slower, I invited them to make any sound that their bodies needed to make and gently vocalize before ending the “journey”. Many of them took a huge sigh and softly hummed. The staff in the room took a while to open their eyes and return to the space. Some were teary, some smiled. They collectively seemed more relaxed and centered. They expressed appreciation of the experience. One nurse stated that, “I feel I now have the strength to continue my day.”
From this example, we can see that the medical team needed a time to process and grieve the sudden loss of their patient. As they were expected to carry on their duties as usual, they may not have otherwise had the opportunity to recognize and process the pain that they were experiencing. Through breath work, visualization, tension release and vocalization, the staff members were able to grieve the loss safely with music and with the music therapist containing the emotions. This music provided safety as they tapped into their inner resources which enhanced their capacity to cope and carry on throughout the rest of the day.
It is cardinal to increase the awareness and recognize the importance in caring for our caregivers. Our team was proactive in taking a lead in introducing this change within our medical culture. Providing supportive mechanisms within the workday can improve the emotional wellbeing of healthcare professionals and potentially prevent compassion fatigue, enhance the quality of patient care, and leading furthermore, to a healthier hospital culture.
Music Therapy Group for Patients and Family Members
Perpetual noise and harsh lighting in a typical hospital environment, coupled with poor nighttime sleep patterns and medication, often contribute to disturbance of inpatient circadian rhythm. As a result, it is common for patients to feel drowsy in the day time. Excessive daytime sleep can continue the vicious cycle of abnormal sleep/wake patterns.
There have been literatures supporting the benefits of engagement in daytime activity and the impact of positive socialization on the improvement of sleep.63,64 The Project Sleep Music Therapy Group was designed to facilitate positive socialization amongst patients and family members. We sought to provide opportunities for patients - who would otherwise be bed bound- to leave their rooms with a structured means to engage in tension-release activities such as group instrumental improvisation, singing and dancing. The music therapy group was initiated as part of Project Sleep and took place in the late afternoon twice a week with the intention of encouraging daytime activity and wakefulness to further promote better sleep at night. Active music-making created a safe venue for the patients to express and release their agitation, anger, and the pent up tension that could be unresolved when confined to a bed.
This group also provided support to anxious and exhausted family members- especially for patient’s children, who are often more susceptible to the stress of the environment and might feel overwhelmed and/or scared of the unknown circumstances illness can render. The following vignette is an example of the music therapy group that addressed the psychosocial needs of the patients while simultaneously provided normalization for the visiting family member’s child.63
Music Therapy Group Case: Patients and Family
(To maintain confidentiality of the individuals, all the names used are pseudo names.)The group consisted of a geriatric patient with dementia, Gail, a middle aged woman, who was the daughter of a patient, Rebecca, and her 5 year-old daughter Jessica. Gail was brought to the group as referred by her aid, Susan, because she was in the hospital for many weeks and Susan felt that Gail needed stimulation and socialization. Gail appeared to have a short attention span and her speech was for the most part incomprehensible. Despite the challenge with communication, I was able to connect with Gail through clinical music improvisation. Gail appeared to listen and immediately smiled and engaged in direct eye contact with me, which was reported by her aid that it rarely occurred outside of the context of our music experience. Although she initially seemed to have a short attention span and would wander around the room, I found that she responded to the Habanera, aria of the French opera ‘Carmen.’ When Gail heard the melody and strong rhythmical patterns created on the keyboard, her eyes brightened and she spontaneously started dancing. It was during this time, Rebecca, the daughter of another patient, and the 5 y/o Jessica entered the lounge. Jessica appeared excited as she entered the room and immediately grabbed a shaker and played along. I engaged all three in instrumental improvisation and ended the group with the girl’s preferred song, which was ‘Wheels on the Bus.’ Rebecca expressed that Jessica had been scared by seeing how sick her grandfather was-(he was sleeping in a room down the hall).
The playful and interactive music-making process provided both Rebecca and Jessica with a healthy and interactive way to release the tension they might have been experiencing at that time. Attending the Music Group restored a sense of play and normalization during her visit, and was a force of creativity leading toward community building for several other patients that later entered the lounge.
Individual Music Therapy: Danielle-Procedure
Medical music psychotherapy66,67,68,69 was offered to individual patients through referral from the medical team. Areas of need in the referral included but are not limited to pain, anxiety, depression, isolation, agitation, need for tension-release, stimulation and socialization.66,67,68,69
(See APPENDIX I for the LACMM music therapy referral form). Each of these areas can precipitate insomnia. The data of the patient surveys reflected that the top 3 reasons for waking at night are nighttime medical routine, pain, and anxiety. Music therapy can address 2 out of these 3 areas. The trust and the therapeutic relationship established between the patient and the therapist is a central key toward improving quality of sleep. Patients need to feel safe enough to relax and let go of the hypervigilance that often can develop during hospitalization.41,56,69,70,71,72 The following example is an individual session whereby music therapy functioned as a catalyst of trust and where the music served as an anchor during a painful procedure, which after the procedure, supported the patient’s transition to sleep.
(The name of the patient and other potentially identifiable information are altered for confidentiality)
Danielle, a middle aged woman, was referred by the nurse manager due to isolation and reports of severe pain. She was on contact precaution in the isolation room and had been in the hospital for a month after having recently been transferred from a neighboring medical unit. Danielle lived alone with limited psychosocial support. She had no children and was estranged from her siblings. She had several medical issues resulting to her frequent hospitalization. The medical staff described her as angry and “nasty” towards anyone entering the room.
Upon my initial entry, Danielle presented as angry, stating: “you guys just leave me here to rot and nobody expletive cares about me.” In listening and acknowledging her frustration, I let her know that she was referred to music therapy to provide her with emotional support and pain management. Danielle’s tone and facial expression softened gradually as I started to improvise gentle arpeggios on the guitar. The chords were consisted of dissonant intervals to match her tension and resolved to consonant chords to facilitate a natural rhythm of tension release. Soon after, a nurse entered the room to change her dressing. He invited me to continue the music during the procedure, as he said it “might be painful.” I continued to improvise gentle tension-release chord progressions in ¾ meter on the guitar as the nurse prepared the equipment. Danielle laid down. Her breathing became rapid and shallow. Noticing this, I began to engage Danielle’s breathing with my vocalization. I sang in descending contours to soothe her and encouraged her to exhale through her mouth and make any sounds that her body needed to make. Danielle responded to the verbal guidance and the pulse of the music and elongated her exhalation through her mouth each time. When the nurse began the treatment, she screamed. I continued the music, increasing the intensity with dynamic and harmonic tension to match her emotional state as she moaned while maintaining the pulse and structure to provide containment and grounding. Responding to Danielle’s moaning, I started to vocalize “ah”, the vowel she chose to express her pain, in descending contours to soothe her and accompany her suffering. Danielle’s body appeared more relaxed as music continued and her moans sounded more rhythmic and communicative. My intuition led me to singing “You Are My Sunshine” and Danielle. immediately cried as I sang. The music and singing continued, serving as emotional containment to her release. She then started to sing “Over the Rainbow” with me and she seemed to become more able to tolerate the pain, evidenced by her facial expression. She engaged in direct eye contact as she sang with me for a while until the procedure was finished. Eventually, she began to close her eyes as I provided gentle holding music to soften the atmosphere of the room. As we closed, she smiled and said “thank you” allowing her body to settle in a comfortable position. I gradually slowed down the music and simplified the music elements42 to elicit deeper relaxation. Danielle transitioned to sleep rapidly as the sedative music continued. She nodded and smiled as she fell asleep.
This is a significant case as it demonstrates how medical music psychotherapy can support pain management. It serves as containment forDanielle’semotional release and is an important catalyst for establishing trust between the patient, her nurse and the therapist. This trust tends to transfer toward not only the hospital experience, but also toward the way in which patients learn to trust their own bodies, which can enhance self- regulation, rather than harvesting fear and anxiety that might perpetuate feelings of being ill or festering dis- ease. From being seemingly angry and feeling threatened toward eventual trust and acceptance, Danielle found the music therapy and my presence to be an anchor for tolerating the pain she experienced during procedural support. The live music and the therapeutic rapport elicited a sense of safety and trust that enabled her to fall asleep soon after the painful medical intervention.
Lullaby Album & Hospital Channel
An ongoing development of Project Sleep involved a team-composed program of lullabies recorded and assembled onto an album for patients on the pilot Project Sleep unit. It was provided eventually throughout the medical center on the broadcast television station. It was produced as an augmentation to the medical music psychotherapy service of Project Sleep, recognizing the need for music in the evening, when the feeling of isolation tends to intensify. The album contains lullabies in 8 languages, including commonly spoken languages in NYC such as English, Spanish, Mandarin, Cantonese, and Hebrew. It is the first relaxation music channeled on patient TV that was designed and created by certified music therapists, integrating clinical understanding and artistic intentions. Because it is available on every patient TV, patients and families are able to access their choice of music at any time. The multicultural nature of the album also addresses the rich diversity amongst a multitude of cultures that comprises the patients in the heart of New York City.
Conclusion
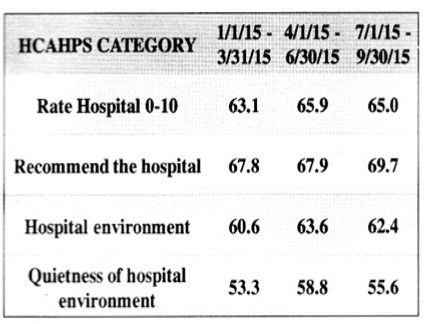
According to the Project Sleep: A Multidisciplinary Quality Improvement Project Poster, 27 the result of Project Sleep rendered from 125 patient surveys demonstrated a significant difference in the mean quality of sleep (pre and post intervention: 2.8 vs 3.34, scale 1-5,p = 0.0003). A trend was also noted of decreased zolpidem orders. There was no significant difference in falls, however, the unit baseline was low. The HCAHPS scores showed a trend of improvement in 4 relevant categories including notably, quietness of the environment.
As a major part of Project Sleep, the music therapy team has provided services to date for approximately 200+ patients. Although there have been numerous studies reporting the use of music to improve quality of sleep in hospitals,9,10,11,12,13,14,15,16,17,18,19,20 there is little on the use of informed interventions of live music therapy by music therapistswho are credentialed to best assess and treat the often traumatic experiences of vulnerable patients. Studies on the use of music to improve sleep 9,10,11,12,13,14,15,16,17,18,19,20 are primarily focused on the use of recorded music and have not considered the importance of the therapeutic relationship that is carefully developed between patients and therapists, which can play a critical role in fostering a strong sense of trust and safety that in turn can effectively foster better sleep. Our comprehensive music therapy model elucidates the capacity of medical music psychotherapy to address the environmental, physical, psycho-emotional, and psychosocial needs that influence patients’ quality of sleep.
The results rendered by Project Sleep demonstrated that, with multidisciplinary collaboration and staff engagement, low cost and easily available interventions can improve quality of sleep and patient experience while avoiding zolpidem use.27 Moreover, the multidisciplinary collaboration and comprehensive music therapy protocol developed for Project Sleep provide outcomes that take an imperative step toward leading a change in medical culture. This change is marked by an initiative necessary for creating a sensitive “healing” environment and a healthier caregiver community, which will fortify our quest to excel in the delivery of a stronger, more personalized patient/customer care delivery system- an environment that will ultimately be perceived by patients and their caregivers as one of care and compassion.
MOUNT SINAI HEALTH SYSTEM
Music Therapy Referral
Name of PT: _________________________________________
Diagnosis: __________________________________________
Floor & Room: ______________________________________
Primary Language of Patient: ____________________English: ___ yes ___ no
Caretaker(s) Name: ____________________________________
Primary Language of Caretaker: __________________English: ___ yes ___ no
Relationship to patient: ____ mother ____ father ____sibling
____ foster parent ____ relative ____ friend
Reason (s) of Patient’s Referral for Music Therapy (definitions on reverse side) Check areas that apply:
Anxiety/Fear:( ) Separation Anxiety( ) Pre or post operative Anxiety ( ) General Anxiety
Pain/Stress:( ) Breathing Difficulties( ) In need of tension release
Expressive Difficulties:( ) Depression or Non-Verbal( ) Acting out or hyperactive
Coping:( ) In Facing the Illness( ) Self Esteem ( ) Communication/Socialization
In Loss of
Consciousness:( ) Increase awareness( ) Increase stimulation or use of imagery
Other Specify: _____________________________________________________________________________
Comments: ________________________________________________________________________________
__________________________________________________________________________________
___________________________________________________________________________________
Person Referring: _______________________________________ Ext: ____________ Date: ______________
MUSIC THERAPY REFERRAL CRITERIA
I. Anxiety/Fear
A. Music Therapy soothes, familiarizes, and/or activates:
B. Separation anxiety Chanting, musical holding and collaborative musical experiences create a feeling of safety in the hospital.
C. Pre/Post operative anxiety Making music relaxes and eases the mind and body of tension and fear stimulated by hospital procedures.
D. General anxietyMusical experiences help patients make sense of their fears through a non-threatening medium.
II. Pain/Stress
A. Clinical improvisation provides an alternative,
B. non-verbal means of release for a patient in discomfort:
C. Breathing & VocalizingLife rhythms and tonal intervallic synthesis help a patient synchronize and deepen the breathing process. Toning stimulates the connection between the body breath and feeling states.
D. Tension releaseOpening channels of musical creativity stimulates the body’s need to release tension.
III. Expressivity
A. Depression, non-verbal/inactivity Structured and unstructured therapies help elicit feelings that may be “muted” or “blocked”.
B. Acting out or hyperactivity The implicit structure music therapy techniques such as African drumming song sensation, and instrumental composition offer patients a safe means of channeling their excessive amounts of energy.
IV. Ego strength/Coping
A. Facing the illness The metaphoric use of music in song selection and composition offer patients a safe way into understanding and adjusting to their illness.
B. Self esteem Performing and tape creating strengthen a patient’s feeling of worth during this fragile time.
C. Communication/Socialization Community singing, drumming circles, and collaborative free improvisations foster communications between patients and within families.
V. Loss of Consciousness/Coma/ICU
A. Awareness The use of familiar melodies help patients become oriented or tuned in to a state grounded, familiarized awareness.
B. Stimulation The use of music and guided imagery stimulates the healing process.
References
- 1. (2006) Institute of Medicine. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem.Washington,DC:TheNationalAcademiesPress.
- 2.(March2015) National Centerfor Chronic Disease Prevention and Health Promotion. Sleep and Sleep Disorders. https://www.cdc.gov/sleep/index.html
- 3.Chan M F, Chan E A, Mok E. (2010) Effects of music on depression and sleep quality in elderly people: A randomized controlled trial. Complement Ther Med;18(3-4):. 150-9.
- 4.Krystal A D.(Dec2006) “Sleep and Psychiatric Disorders: Future Directions,”. , Psychiatric Clinics of North America; 29(4), 1115-30.
- 5.Ford D E, Kamerow D B. (1989) Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention?. , JAMA; 262, 1479-1484.
- 6.Roberts R E, Shema S J, Kaplan G A, Strawbridge W J. (2000) Sleep complaints and depression in an aging cohort: a prospective perspective. , Am J Psychiatry; 157, 81-88.
- 7.Cheatle M D, Foster S, Pinkett A, Lesneski M, Qu D.Assessing and Managing Sleep Disturbance. in Patients with Chronic Pain. Sleep Medicine Clinics, Volume 11, Issue 4 531-541.
- 8.Alsaadi S M, McAuley J H, Hush J M, Maher C G. (2011) Prevalence of sleep disturbance in patients with low back pain. , European Spine Journal 20, 737-743.
- 9.Johnson J E. (2003) The use of music to promote sleep in older women. , J Community Health Nurs; 20(1), 27-35.
- 10.Jespersen K V, Koenig J, Jennum P, Vuust P. (2015) Music for insomnia in adults. Cochrane Database Syst Rev;8:CD010459.
- 11.Chen C K, Pei Y C, Chen N H. (2014) Sedative music facilitates deep sleep in young adults. , J Altern Complement Med; 20(4), 312-17.
- 12.Chi G C, Young A. (2011) Selection of music for inducing relaxation and alleviating pain: literature review. Holist Nurs Pract;. 25(3), 127-35.
- 13.Lai H L, Good M. (2004) Music improves sleep quality in older adults. , J Adv Nurs; 53(1), 134-44.
- 14.Shum A, Taylor B J, Thayala J, Chan M F. (2014) The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complement Ther Med;. 22(1), 49-56.
- 15.Shaw R. (2016) Using music to promote sleep for hospitalized adults. , Am J Crit Care; 25(2), 181-4.
- 16.Chang E T, Lai H L, Chen P W, Hsieh Y M, Lee L H. (2012) The effects of music on the sleep quality of adults with chronic insomnia using evidence from polysomnographic and self-reported analysis: A randomized control trial. , Int J Nurs Stud; 49(8), 921-30.
- 17.Hu R F, Jiang X Y, Hegadoren K M, Zhang Y H. (2015) Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. , Crit Care; 19, 115.
- 18.Evans D. (2002) The effectiveness of music as an intervention for hospital patients: a systematic review. , J Adv Nurs; 37(1), 8-18.
- 19.Blanaru M, Bloch B, Vadas L. (2012) The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn;4(2):e13.
- 20.Ryu M J, Park J S, Park H. (2012) Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. , J Clin Nurs;21(5-6): 728-35.
- 21.Su C P, Lai H L, Chang E T, Yiin L M, Perng S J et al. (2013) A randomized controlled trial of the effects of listening to non-commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care units. , J Adv Nurs; 69(6), 1377-89.
- 22.Foley D, Monjan A, Brown S. (1995) Sleep complaints among elderly persons: an epidemiologic study of three communities. , Sleep; 18, 425-32.
- 23.Foreman M, Wykle M.the NICHE Faculty (1999)Sleep disturbances in elderly patients.In:Mezey M, ed.Geriatric nursing protocols for best practice.NewYork:Springer Publishing Company,P. 13-25.
- 25.Bryant P A, Trinder J, Curtis N. (2004) Sick and tired: does sleep have a vital role in the immune system?. , Nat. Rev. Immunol 4, 457-467.
- 26.Majde J A, Krueger J M. (2005) Links between the innate immune system and sleep. , J. Allergy Clin. Immunol 116, 1188-1198.
- 27.Grabscheid E, Brodt Z N, Perry H, Tapper C, Gallagher M A et al. (2016) Project Sleep: A Multidisciplinary Quality Improvement Project. Mount Sinai Beth Israel, Icahn School of Medicine. , New York, NY;
- 28.Zaubler T S, Murphy K, Rizzuto L, Santos R, Skotzko C et al. (2013) Quality improvement and cost savings with multicomponent delirium interventions: replication of the hospital elder life program in a community hospital. The Academy of Psychosomatic Medicine.ElsevierInc;. 54, 1492-1499.
- 29.Inouye S K, Baker D I, Fugal P, Bradley E H. (2016) Dissemination of the hospital elder life program: implementation, adaptation, and successes. The American Geriatric Society. 54, 1492-1499.
- 30.Nagel C L, Markie M B, Richards K C, Taylor J L. (2003) Sleep promotion in hospital elders. MEDSURG Nursing. 12(5), 279-290.
- 31.LaReau R, Benson L, Watcharotone K. (2008) Examining the feasibility of implementing specific nursing interventions to promote sleep in hospitalized elderly patients. Geriatric Nursing. 29(3), 197-206.
- 32.Rostata J R, Dunn M, Phelan G, Braun C, Chiu C T et al. (2015) Implementing an evidence-based sleep protocol to reduce falls on an inpatient rehab unit: an interdisciplinary approach. , Department of Nursing & Patient Care Services, Mount Sinai St. Luke’s,NewYork,NY
- 33.Alessi C A, Martin J L, Webber A P, Kim E C, Harker J O et al. (2005) Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. , Journal of the Ameican Geriatric Society 53(5), 803-810.
- 34.Rossetti A, Canga B. (2013) Environmental music therapy: rationale for ‘multi-individual music psychotherapy’ in modulation of the pain experience.In: MondanaroJ,Sara GA, eds.Music and Medicine: Integrative Models in the treatment of Pain.SatchnotePress. , New York, NY 276-294.
- 35.Canga B, Hahm C L, Luciso D, Grossbard M L, Loewy J V. (2012) Environmental music therapy: a pilot study on the effect of music therapy in a chemotherapy infusion suite. , Music and Medicine; 4(4), 221-230.
- 36.Stewart K, Schneider S. (2007) The effect of music therapy on the sound environment in the neonatal intensive care unit: a pilot study.In Loewy J.ed.Music Therapy in the Neonatal Intensive Care Unit.Satchnote Press,New. , York, NY: 85-100.
- 37.Hweidi I M. (2007) Jordanian patients’ perception of stressors in critical care units: a questionnaire survey. , I J Nur Stud; 44(2), 227-235.
- 38.Rabat A, Bouyer J J, Aran J M, LeMoal M, Mayo W. (2005) Chronic exposure to an environmental noise permanently disturbs sleep in rats: inter-individual vulnerability. , Brain Research; 1059(1), 72-82.
- 39.Porges S W. (2011) The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. , New York: Norton;
- 40.Maschke C. (2003) Stress hormone changes in persons exposed to simulated night noise. Noise Health. 5(17), 35-45.
- 42.BA van der Kolk. (2014) . The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma.PenguinGroupLLC(USA) .
- 43.dP Vianna, Cardoso A, Rodrigues. (2015) Noise pollution and annoyance: an urban soundscapes study. Noise Health. 17(76), 125-33.
- 44.Goines L, Hagler L. (2007) Noise pollution: a modern plague. , Southern Medical Journal; 100(3), 287-294.
- 45.Stansfeld S A, Matheson M P. (2003) Noise pollution: non-auditory effects on health. , British Medical Bulletin 68, 243-257.
- 47.Ising H, Kruppa B. (2004) Health effects caused by noise: evidence in the literature from the past 25 years. Noise Health. 6(22), 5-13.
- 48.Spreng M. (2000) Possible health effects of noise induced cortisol increase. Noise & Health. 2(7), 59-63.
- 49.Prasher D. (2009) Is there evidence that environmental noise is immunotoxic? Noise & Health. 11(44), 151-155.
- 50.Pascuan C G, Uran S L, Gonzalez-Murano M R, Wald M R, Guelman L R et al.( 2014Jan-Mar )Immune alterations induced by chronic noise exposure: comparison with restraint stress in BALB/c and C57BI/6mice.JImmunotoxic;. 11(1), 78-83.
- 51.Cabrera I N, MHM Lee. (2000) Reducing noise pollution in the hospital setting by establishing a department of Sound: A survey of recent research on the effects of noise and music in Health Care. Preventive Medicine. 30, 339-345.
- 52.Abendroth M, Flannery J. (2006) Predicting the risk of compassion fatigue: A study of hospice nurses. Journal of Hospice and Palliative Nursing. 8(6), 346-356.
- 54.Aycock N, Boyle D.(April2009) Interventions to manage compassion fatigue in oncology nursing. , Clinical Journal for Oncology Nursing; 13(2), 183-191.
- 55.Adams R E, Boscarino J A, Figley C R. (2006) Compassion fatigue and psychological distress among social workers: A validation study. , Am J Orthopsychiatry; 76(1), 103-108.
- 56.Coetzee S K, H C Klopper. (2010) Compassion fatigue within nursing practice: A concept analysis. Nursing and Health Sciences. 12, 235-243.
- 57.Figley C. (1995) Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. , New York, NY: Brunner-Routledge
- 58.Figley C. (2002) Compassion fatigue: Psychotherapists’ chronic lack of self-care. Psychotherapy in Practice. 58(11), 1433-1441.
- 60.Sabo B. (2011) Reflecting on the concept of compassion fatigue. , The Online Journal Issues in Nursing 16-1.
- 61.Loewy J, Hara A F. (2007) Caring for the Caregiver: The Use of Music and Music Therapy in Grief and Trauma. American Music Therapy Association, Inc.
- 62.F Bosco Daring, Dread Discharge, Delight. (2007) In Loewy J, Hara AF (Eds.).Caring for the caregiver:The use of music and music therapy in grief and trauma. American Music TherapyAssociation,Inc.
- 63.Ledger A J, Baker F A. (2007) An investigation of long-term effects of group music therapy on agitation levels of people with Alzheimer’s Disease. , Aging & Mental Health 11(3), 330-338.
- 64.Huang H W, Huang C B, Chang Y H, Wu Y P, Wu C J et al. (2012) A study of the relationship between music therapy and sleep quality in old patients. , International Journal of Evidence-Based Healthcare; 10(3), 259-259.
- 65.Loewy J. (2013) Respiratory care for children. In Bradt (Ed.). Guidelines for music therapy practice pediatric care:Gilsum,NH:BarcelonaPublishers;. 403-441.
- 66.Loewy J, Scheiby B. (2001) Developing the culture of music psychotherapy in the medical setting. Paper presented at The Evening Lecture Series atNewYorkUniversity/Nordoff-Robbins Center for Music Therapy.May.NewYork,NY.
- 67.Loewy J. (2000) Music psychotherapy assessment. , Music Therapy PerspectivesAmerican Music Therapy Association, Inc.; 18(1), 47-58.
- 68.Loewy J, Dileo C. (1999) The use of music psychotherapy in the treatment of pediatric pain. Music Therapy & Medicine: Theoretical and Clinical Applications;. 189-205.
- 69.Loewy J. (2007) Developing music therapy programs in medical practice and healthcare communities.In J Edwards(Ed.),Music:Promoting health and creating community in healthcare contexts. Cambridge,UK:Cambridge Scholars Press:. 17-28.
Cited by (13)
This article has been cited by 13 scholarly works according to:
Citing Articles:
Journal of Sleep And Sleep Disorder Research (2024) Crossref
Journal of Sleep And Sleep Disorder Research (2024) OpenAlex
LA Nussbaum, TM Janjua, J. Pederson, ES Nussbaum - Journal of Sleep And Sleep Disorder Research (2024) Semantic Scholar
Journal of Pain Research (2022) OpenAlex
Journal of Pain Research (2022) Crossref
Samuel N. Rodgers-Melnick, Lucas Lin, K. Gam, Evanilda Souza de Santana Carvalho, C. Jenerette et al. - Journal of Pain Research (2022) Semantic Scholar
Brain Sciences (2022) Crossref
Brain Sciences (2022) OpenAlex
J. Loewy - Brain Science (2022) Semantic Scholar
Journal of Pain and Symptom Management (2021) Crossref
BMJ Open (2021) Crossref
BMJ Open (2021) OpenAlex
Lixia Chen, Fang Wang, Jianhua Li, Li Cui, Xiaoli Liu et al. - BMJ Open (2021) Semantic Scholar
Nature and Science of Sleep (2020) OpenAlex
J. Loewy - Nature and Science of Sleep (2020) Semantic Scholar
Journal of Pain and Symptom Management (2020) OpenAlex
John Mondanaro, Gabriel A Sara, Roshni Thachil, Marija Pranjić, Andrew Rossetti et al. - Journal of Pain and Symptom Management (2020) Semantic Scholar
Journal of Sleep And Sleep Disorder Research (2018) OpenAlex