Abstract
The benefits of exclusive breastfeeding are well-known. Despite the legislative and systemic efforts to promote breastfeeding in South Korea, the nation’s current rate of exclusive breastfeeding (5.2%) during the infant’s first six months is alarming. Under the framework of the theory of planned behavior (TPB), this study elicited the beliefs around exclusive breastfeeding commonly held by low-income women participating in NutriPlus, the community nutrition program. Using a convenient sampling method, online open-ended surveys were conducted with two program clinics in Seoul during spring of 2024. The survey included questions about their demography and beliefs regarding indirect theoretical constructs of the exclusive breastfeeding behavior by listing top three things that came to their mind. A total of 120 NutriPlus clients participated in this survey. Though 53.1% of postpartum women were breastfeeding, only 28.1% were breastfeeding exclusively. Based on most frequently mentioned beliefs, we classified them to behavioral, normative, and control beliefs under TPB. Modal behavioral beliefs were healthy babies (n=87) and mother-baby bonding (n=71) and feeding issues (n=96) and inconvenience resulting from the act of breastfeeding (n=86). Family members seemed to shape both positive (n=122) and negative (n=37) normative beliefs. The presence of support (n=84) mattered to facilitate breastfeeding, while feeding issues (n=98) played as barriers. Promotion efforts need to emphasize breastfeeding knowledge and skill building and include family members and society at large to improve the awareness and transform barriers of breastfeeding to facilitators.
Author Contributions
Academic Editor: Loai Aljerf, Department of Life Sciences, Faculty of Dentistry, University of Damascus
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2025 Yeon Bai, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Breast milk provides the infant with necessary nutrients needed during important stages in growth and development 1. Breastfeeding has shown to increase cognitive development, learning and education attainment, and productivity which in the future can help lead to increased wages and better economy 2. Breastfeeding also has health benefits for the mother, including a decreased risk for breast and ovarian cancers, and postpartum mental health issues 3. The World Health Organization (WHO) alongside the United Nations International Children’s Emergency Fund (UNICEF) have a global recommendation for newborns to be breastfed starting within the first hour of birth and continuing with exclusive breastfeeding for at least six months 4. Yet, the early termination of breastfeeding is prevalent across the nations. Globally 48% of infants under six months were exclusively breastfed in 2023 5.
In South Korea, the breastfeeding initiation rate within the first hour of birth is 52.4% 6, yet the current rate of exclusive breastfeeding at six months is 5.2 %, far below the goal of the 40% exclusive breastfeeding rate by 2030 set by the Korean Ministry of Health and Welfare 7, 8. The failure to meet this goal is not necessarily due to the lack of effort. The Korean government has been encouraging breastfeeding through legislation and initiatives, e.g., the National Parental Leave Policy 9, the Act on Equal Employment for Men and Women Support for Work-Family Balance 10, and ongoing education on breastfeeding initiatives. However, these efforts have not proven to lead to a longer duration of breastfeeding or its exclusivity.
Formula companies employ aggressive marketing strategies and downplay the benefits of human milk feeding by making nutritional claims of formula as an equal or better source of nutrition for an infant, hence driving down the rate of exclusive breastfeeding 11. In developed countries, where formula is more widely available and affordable, women tend to elect to feed their infants with formula instead of mother’s own milk, hence leading to lower exclusive breastfeeding rates for the recommended six months than other countries 12, 13. The low breastfeeding rate in South Korea could be due in part to its becoming a high-income developed country in recent decades 14.
While the country has elevated its global economic standing, about 15% of the South Korean population is living in poverty as of 2020 15. Korea’s current poverty rate is alarming as it is almost twice as high as the current global poverty rate at 8.5% 16. The NutriPlus program in South Korea was established in 2005. This program targets low socioeconomic class families focusing on providing nutrition education along with supplemental foods to improve nutrition knowledge, attitude, and dietary behaviors. The program offers group lessons, individual counseling sessions, and home visits as well as breastfeeding promotion 17. Breastfeeding challenges faced by low socioeconomic class families need to be explored to increase the breastfeeding duration and exclusivity for all populations in Korea.
In this study, we aimed to examine the individual and social norms regarding the act of breastfeeding among low-income families within the Korean community. Specifically, we framed the study under the theory of planned behavior and explored underlying beliefs around exclusive breastfeeding for the first six months of an infant’s life among women participating in the NutriPlus program.
Theory of Planned Behavior
The theory of planned behavior depicts that behavior is goal driven. Behavior can be traced back to intention and then further back to beliefs towards a behavior. The theory explains that a behavior is the outcome of a series of other constructs including intention, attitude, subjective norm, and perceived behavioral control. To understand why people behave the way they do, we need to look back at the beliefs underlying each construct. People perform a behavior when they want to perform that behavior (intention). The intention is formulated by the combination of three constructs i.e., positive attitude toward, subjective norm of, and perceived behavioral control of performing the behavior. These constructs in turn are driven by belief domains (indirect constructs): attitude by behavioral beliefs, subjective norm by normative beliefs, and perceived behavioral beliefs by control beliefs. Behavioral beliefs are determined by the reasoning of if performing the behavior is an advantage or disadvantage to the performer. Normative beliefs are whether performing the behavior is approved or disapproved by others. Control beliefs are looking at facilitators and barriers of performing the behavior 18.
Materials and Methods
Study Design
This cross-sectional study using online survey was designed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. The study was conducted with NutriPlus program clients in South Korea. In spring of 2024, researchers contacted two NutriPlus programs housed in public health centers in the northern district of Seoul to recruit study participants. Eligible criteria for participation were 18 years of age and over, being a woman, and current participation in one of the two selected NutriPlus programs. This study included only woman gender because the target population is NutriPlus program participants and the NutriPlus program was designed for pregnant or postpartum women, infants, and children under age 66 months. In May of 2024, staff of the two public health centers assisted with study participant recruitment by posting the recruitment message to their communication systems. The informed consent forms were obtained from all participants before the survey. The survey procedures and protocols were approved by the Institutional Review Board of Montclair State University (IRB No. IRB-FY-22-23-2818). The link to the survey was embedded in the recruitment message. Participants were incentivised by having offered a chance to win a raffle by completing the survey. Data collection was completed by June of 2024.
Survey Instrument
A set of demography questions to provide the context of the data included age, NutriPlus enrollment duration, breastfeeding experience, and timing of breastfeeding termination, education, and working status. Framed under the theory of planned behavior, salient beliefs regarding exclusive breastfeeding for the first six months of life were elicited using open-ended questions. Salient beliefs relating to direct constructs of the theory, i.e. attitude toward, subjective norm and perceived behavioral control of the behavior, include behavioral, normative, and control beliefs. Salient beliefs were measured by asking NutriPlus participating women about feelings and opinions regarding exclusive breastfeeding for the first six months of life. The elicitation procedure was essential to determine the top-of-the-mind or salient consequences, referents, and circumstances that formed the belief structure underlying the exclusive breastfeeding behavior for six months. To that end, respondents were asked to list the top three things that came to their mind for six open-ended questions.
Data Analysis
The research team members have diverse experience ranging from working with clients or designing community nutrition programs in the U.S. and Korea to conducting nutritional epidemiological studies globally. They have different professional background in nutrition and public health, which helped bring diverse prospectives in study development and result interpretation. At all stages of the study, we employed critical analysis including in questionnaire development and refinement to reduce any potential bias.
The demography data were summarized using a descriptive analysis. Content analyses were performed to extract themes and to identify most frequently mentioned salient beliefs. Responses to open-ended questions were carefully reviewed to select five to ten most frequently mentioned items as the salient set. The responses were then consolidated into behavioral, normative, and control beliefs. Research team members completed each step of the analysis independently and then met to discuss their findings and reached a consensus among team members on final sets of salient beliefs. Responses were tallied to determine modal and popular responses for each belief.
Results
A total of 120 NutriPlus clients participated in this study. The mean age of participants was 34.5 ± 4.5 years old and the mean duration of participation was 9.8 ± 10.7 months. Among postpartum women under 12 months post-delivery, 53.1% were breastfeeding to some degree: exclusive (28.1%) or partial (25%). Most participants (38.5%) were enrolled in the child (over 12 months of age) category. Nearly half of the study participants (48.7%) recently (less than six months ago) joined the NutriPlus program. (Table 1)
Table 1. Study Participant Characteristics| Category | Frequency (N=120) | Relative Frequency (%) |
| NutriPlus Participation Category | ||
| Pregnant | 7 | 6.0 |
| Postpartum women | Beliefs about exclusive breastfeeding | |
| exclusive breastfeeding | 9 | 7.7 |
| no breastfeeding | 15 | 12.8 |
| mixed feeding | 8 | 6.8 |
| Child, over 12 months old | 45 | 38.5 |
| Infant | ||
| exclusive breastfeeding | 11 | 9.4 |
| fully formula feeding | 11 | 9.4 |
| mixed feeding | 11 | 9.4 |
| Duration of NutriPlus Participation | ||
| Less than 6 months | 58 | 48.7 |
| 6 months ≤ duration < 1 year | 37 | 31.1 |
| 1 year ≤ duration < 2 years | 17 | 14.3 |
| 3 years or more | 7 | 5.9 |
| Breastfeeding Experience | ||
| Never breastfed | 10 | 8.3 |
| Had breastfed before | 74 | 61.7 |
| Currently breastfeeding | 36 | 30.0 |
| Time Lapse since termination ofbreastfeeding | ||
| Less than or equal to 1 year | 45 | 60.8 |
| 1 year < lapse < 2 years | 9 | 12.2 |
| 2 years < lapse < 3 years | 4 | 5.4 |
| more than 3 years | 16 | 21.6 |
| Education | ||
| High School Grads | 28 | 23.3 |
| 2-year, 3-year, 4-year college grads | 64 | 53.3 |
| Higher than College grads | 28 | 23.3 |
| Student Status | ||
| Part-time Student | 3 | 2.5 |
| Full-time Student | 1 | 0.8 |
| Not a student | 116 | 96.7 |
| Employment Status | ||
| Part-time (Less then 30 hours per week) | 18 | 15.0 |
| Full-time (30 or more hours per week) | 29 | 24.2 |
| No employment | 73 | 60.8 |
The summary of behavioral, normative, and control beliefs mentioned most frequently by participants are shown in Table 2. We assorted specific consequences (advantages/disadvantages), social referents (approvers/disapprovers), and circumstances (facilitators/barriers) of performing the behavior (exclusively breastfeeding for the first six months) under behavioral, normative, and control beliefs, respectively. The most frequently mentioned advantageous consequences of the behavior were healthy babies (n=87), followed by bonding between mother-baby dyad (n=71). Feeding issues (n=96) including insufficient breast milk supply, poor feeding technique, and feeding pain were most common disadvantages mentioned, followed by inconvenience brought by the behavior (n=86) including sleep deprivation, fatigue, and outing challenges. Family members were mentioned most frequently as approvers but also noted as disapprovers of the behavior: as approvers (n=122) vs. disapprovers (n=37). The modal response to disapprovers of the behavior was no one (n=65). Supports (n=84) from workplace, society, and family facilitated the behavior most, followed by the women themselves (n=66), e.g., her own will, breastfeeding knowledge, and her health condition. Most popular barrier of the behavior mentioned was related to feeding issues (n=98), e.g., insufficient milk supply, mother’s poor feeding skills, and baby’s refusal and sucking difficulty.
Table 2. Identified salient consequences, social references, circumstances that were classified into behavioral, normative, and control beliefs| Theoretical Indirect Constructs | Frequency | Relative Frequency (%) |
|---|---|---|
| Consequences (Behavioral Beliefs) | ||
| Advantages (n=316) | ||
| Baby’s health | 87 | 27.5 |
| Mother-baby bonding | 71 | 22.5 |
| Feeding convenience | 61 | 19.3 |
| Economy of finance and time | 35 | 11.1 |
| Baby’s nutrition | 30 | 9.5 |
| Mother’s health | 23 | 7.3 |
| Baby’s development | 9 | 2.8 |
| Disadvantages (n=247) | ||
| Feeding concerns | 44 | 18.3 |
| Mother’s physical condition | 44 | 18.3 |
| Outing challenges | 36 | 14.9 |
| Feeding pain and difficulty | 32 | 13.3 |
| Mother’s diet balance, restricted medication | 29 | 12.0 |
| Mother’s freedom loss | 21 | 8.7 |
| Lack of feeding skills | 20 | 8.3 |
| Responsibility solely rests on mothers | 15 | 6.2 |
| Social Referents (Normative Beliefs) | ||
| Approvers (n=178) | ||
| Family members | 85 | 48.0 |
| Husband | 37 | 20.9 |
| Healthcare Providers | 25 | 14.1 |
| Others (peer mothers, coworkers/friends, elders) | 25 | 14.1 |
| No one | 5 | 2.8 |
| Disapprovers (n=146) | ||
| No one | 65 | 41.7 |
| Others (coworkers/friends, formula companies) | 37 | 23.7 |
| Family members | 24 | 15.4 |
| Lack of self-will | 17 | 10.9 |
| Husband | 13 | 8.3 |
| Circumstances (Control Beliefs) | ||
| Facilitators (n=210) | ||
| Mother’s and baby’s feeding skill | 36 | 17.1 |
| Family support | 35 | 16.7 |
| Self-will, intention, goals | 33 | 15.7 |
| Workplace support | 29 | 13.8 |
| Mother’s milk supply | 24 | 11.4 |
| Mother’s physical condition | 21 | 10.0 |
| Societal support | 20 | 9.5 |
| Mother’s feeding knowledge | 12 | 5.7 |
| Barriers (n=248) | ||
| Feeding challenges | 81 | 21.7 |
| Mother’s emotional/physical condition | 51 | 20.6 |
| Lack of family support | 35 | 14.1 |
| Returning to work | 30 | 12.1 |
| Lack of societal support | 20 | 8.1 |
| Baby’s feeding difficulty | 17 | 6.9 |
| Lack of self-will and intention to breastfeed | 9 | 3.6 |
| Lack of support from healthcare providers | 5 | 2.0 |
Further, each salient belief generated several high-level concepts (overarching themes and categories) under which we could classify specific consequences, social referents, and circumstances as shown in Figure 1. For example, advantages of exclusive breastfeeding for six months drew three high-level concepts noting baby (n=126), mother (n=119), and dyad mother relevant (n=71). Likewise, three themes under disadvantages, i.e., feeding issues (n=96), inconvenience (n=86), and life limitation (n=65), four categories each under approvers and disapprovers of the behavior, three and four themes under facilitators and barriers of the behavior, respectively, emerged.
Figure 1.High level concepts emerged from elicited participants’ beliefs regarding exclusive breastfeeding for the first six months of infant’s life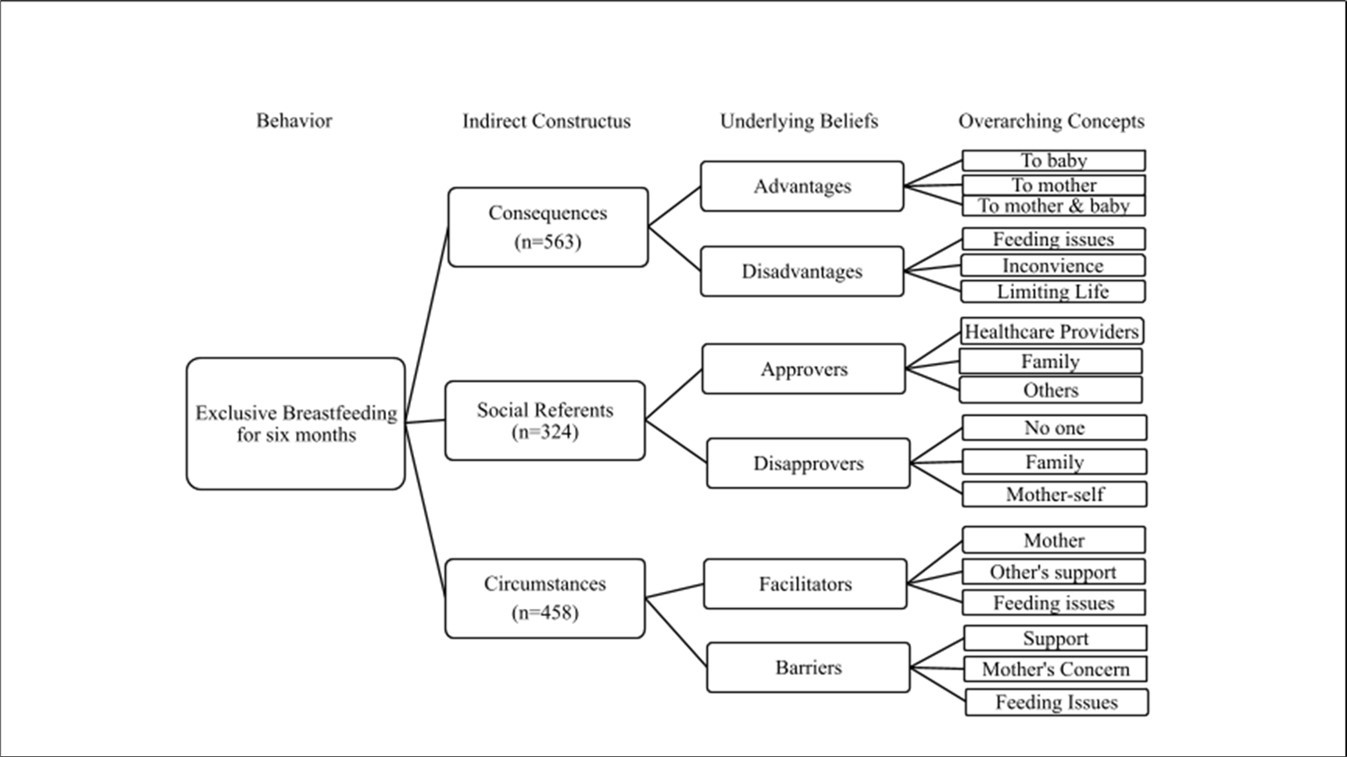
Discussion
The strength of this study is in investigating salient beliefs of the NutriPlus participants in South Korea regarding exclusive breastfeeding for the first six months of the infant’s life.
Identifying the underlying beliefs has never been done with this population in Korea to the best of our knowledge. It is crucial to examine the salient and underlying beliefs to design effective interventions and promotion campaigns to encourage or modify the behavior. According to the theory of planned behavior, tracing back to and addressing specific beliefs held by the target population would highly likely help population formulate positive attitude toward, subjective norm of, and perceived behavioral control of the behavior, which ultimately would lead to the intention to perform the behavior, exclusive breastfeeding for the first six months.
When participants of this study were asked about the advantage of performing the behavior, they considered it from two perspectives, i.e., mother’s and babies’. They highly valued the health benefits for the baby yet appreciated the convenience of nursing and cost savings for the mother, e.g., easy preparation of feeding and being able to respond promptly to baby’s hunger cues. It is reported that breastfeeding is valued for its convenience due to ready-to-feed nature anytime and anywhere 19 and cost-effectiveness, with an estimation of $1,000 or more savings per year 20.
Most of all, women cherished the mother-baby dyad bonding stemming from nursing. These benefits are well recognized in other literature. Modak and others 21 reported profound psychological benefits of breastfeeding resulting from the interplay of oxytocin and prolactin, the foundational hormones during lactation. Oxytocin is released during skin-to-skin contact and lactation, thus fosters a deep emotional connection and forms a secure and nurturing relationship between the mother and the baby, consequently enhancing mother’s and baby’s overall emotional well-being 22. Prolactin supports the role of oxytocin and contributes to postpartum mood regulation, thus influencing maternal bonding behaviors 23.
Women in this study recognized that breastfeeding had helped postpartum recovery, e.g., uterus contract, postpartum bleeding reduction, and postpartum weight loss. Oxytocin along with prolactin facilitates uterus involution after birth in addition to their role in milk production and ejection, the process of which was elucidated in the literature 24. The positive relationship of breastfeeding with postpartum weight loss has been reported in various studies 25, 26, 27, for which women in the study recognized it as an advantage of breastfeeding.
Participants hardly perceived the act of breastfeeding as a pure disadvantage. Instead, the circumstances or situations unhelpful to performing the behavior were viewed as disadvantages. In other words, salient beliefs regarding disadvantages of breastfeeding were closely related to the barriers participants described in this study. Participants were likely to initiate and continue breastfeeding as long as the barriers were removed/alleviated, or circumstances were made to be conducive to the action of breastfeeding.
When assessing the mother’s perceived disadvantages, facilitators, and barriers of the behavior, concerns related to feeding marked the top of the list. Feeding concerns ranged from physiological and technical issues to resultant difficulties stemming from the action of breastfeeding. For example, perceived barriers to breastfeeding included the lack of mother’s and baby’s skills in breastfeeding, either simply mechanical including nipple shape, tongue-tied, nursing position, or complex like uncertainty due to inexperience in breastfeeding, e.g., self-doubt regarding proper feeding intervals or the amount of their own breast milk production etc. These feeding concerns tamper with the behavior and weakens women’s confidence in breastfeeding success.
Nagel and others reported that mother’s psychological distress related to postpartum depression and anxiety could interfere with optimal function of oxytocin and may lead to breastfeeding dissatisfaction or failure 28. This fear and anxiety surrounding infant feeding can cause issues including perceived lack of milk production, baby’s weight gain concerns, improper feeding techniques i.e., breast latching challenges and pain during breastfeeding, and even the pressure to exclusively breastfeed. These factors could ultimately compromise the mother’s self-confidence and create stress as a new mother 29 hindering the overall breastfeeding behavior. Another study reported that the mother’s inner conflict between her own intention and actual practice of breastfeeding could bring on maternal psychological distress, resulting in undesirable breastfeeding outcomes 30.
It is interesting that the high-level concepts of both facilitators and barriers are interconnected: mother’s concerns, feeding issues, and support. In other words, when barriers were resolved they played as facilitators. To transform the perceived barriers to facilitators, lactation and health care providers should work together with expectant mothers beginning at the prenatal period. Studies reported the importance of hospital practice after the delivery 31, 32, 33.
During peripartum period, educations to enable mothers to practice good nursing positioning and guide proper latching as well as rooming-in and immediate skin-to-skin contact practices at hospitals are important and shown to have a positive impact on breastfeeding outcomes 34, 35. Patil and others reported in a systematic review that the lack of breastfeeding education and promotion by hospital staff were barriers to breastfeeding 36. Currently there is minimal education of breastfeeding in schools and hospitals in South Korea. When a baby is born, there is typically less than fifteen minutes of breastfeeding counseling given to the mother, and in some cases this counseling comes at an additional cost 37.
In this study, participants stated that the hospital practices were not conducive to breastfeeding for various reasons including no rooming-in during hospital stay. Interestingly rooming-in was no longer a common practice in South Korea partially due to the recent termination of Baby-Friendly Hospital initiatives (BFHI) in 2023 after over 30 years of implementation certifying 15 Baby-Friendly hospitals. Hospitals were certified as Baby-Friendly based on their ability to mentor new parents and assist in increasing the exclusive breastfeeding duration. The termination of BFHI hampered the nationwide effort to build a system to promote breastfeeding 38.
In Korean culture, it is common that postpartum mothers enter a postpartum care center after their hospital discharge to facilitate their recovery and infant-care education 6. As of 2024, the utility of postpartum care centers was 85.5% nationwide with an average of 12.6 days of stay at the center, showing an increase from 75.1% utility in 2018 6. According to the recent nationwide survey on postpartum care practice 6, breastfeeding education was part of routine care in the center, but rooming-in was only during the feeding time, averaging 3.6 hours of breastfeeding per day. Postpartum women considered the rooming-in practice in the center as a means to building mother-baby dyad (54.9%) and often viewed the rooming-in practice unnecessary (93.1%). Given the prevalence of postpartum care center utility in Korean communities, the lactation educators should seize this opportunity to educate women and help navigating breastfeeding challenges during their stay in the center, typically the first two weeks of post-delivery. Empowering women with breastfeeding skills and knowledge including nursing position and supply-demand mechanism of milk production 39, 40 could improve their breastfeeding self-efficacy and lead to successful breastfeeding and breastfeeding exclusivity.
It is noteworthy that family members were considered both approvers and disapprovers of breastfeeding. Women in this study who worked part- or full-time stated that the workplace breastfeeding support was a facilitator and lack of it was a barrier to breastfeeding. This reiterates the importance of support from workplace and family members, especially husbands.
Physical and mental stress resulting from labor of nursing, burden of house chores, or outing challenges negatively influenced the will of the mother to continue breastfeeding. Therefore, the division of the infant care/feeding and housework responsibility between family members and mothers is essential to relieve the breastfeeding mothers’ physical and mental overload. Societal level supports could entail an awareness campaign regarding functional lactation rooms throughout the town and have them accessible to breastfeeding women, which facilitates easy outings and lessens the notion of mother’s being tied down with the infant.
The sampling was geographically confined in one district in the city, which may have influenced the diversity of the opinions. The use of the term exclusive breastfeeding in Korea included not only breast milk feeding exclusively, water and other fluid use combined with breast milk, but also breast milk feeding with small amount of solid food. This limited our ability and the resources to identify the accurate exclusive breastfeeding rate in Korea. In the future there may be a need to clearly differentiate between full, exclusive, and complementary breastfeeding, as the terms are often used interchangeably. This practice complicates the accurate measurement of exclusive breastfeeding rates. In addition, further studies are needed to examine how beliefs about breastfeeding evolve over time, which will help in designing and modifying promotion campaigns to achieve better breastfeeding outcomes. Innovative strategies are required to design interventions that can transform existing barriers into facilitators, creating a more supportive environment for breastfeeding and ensuring its exclusivity. Ongoing monitoring of the effectiveness of these intervention programs by organizations such as local governments, public health centers, and postpartum care centers is essential to maintain the integrity of the programs and ensure their continued success.
Conclusion
Medical and lactational interventions, along with lactation education during pregnancy and post-delivery, can help alleviate barriers to breastfeeding. Promotion efforts should build on women’s existing knowledge of the benefits of breastfeeding to address any challenges they may encounter on the path to successful breastfeeding. Creating a supportive environment that counters perceived barriers and highlights facilitators will be crucial for the success of breastfeeding promotion efforts in South Korea.
Conflict of Interest
The authors have no conflict of interest to disclose.
Acknowledgements
This study was partially supported by internal research grant from Montclair State University, Shingu College (Faculty Professional Competency Reinforcement Program, 2024-KYO008), and Seoul National University. Authors would like to thank the participants of this study for their time, Jamie Watt for manuscript editing, community nutrition program staff and Dr. Jihyun Yoon for their support to launch this study in South Korea.
References
- 1.Alimoradi F, Javadi M, Barikani A, Kalantari N, Ahmadi M. (2014) An Overview of Importance of Breastfeeding. J Compr Pediatr [Internet]. cited
- 2.Wallenborn J T, Levine G A, A Carreira Dos Santos, Grisi S, Brentani A et al. (2021) Physical Growth, and Cognitive Development. Pediatrics. 147(5), 2020008029.
- 4. (2024) World Health Organization [Internet]. [cited. Breastfeeding. Available from:https://www.who.int/health-topics/breastfeeding
- 6.Whang O K, Kim J Y, Yoo H mi, Lee Y J, Yang M S et al. (2024) Postpartum Care Survey [Internet]. Ministry of Health and Welfare;. Available from:https://www.mohw.go.kr/board.es?mid=a10411010100&bid=0019&act=view&list_no=1484554&tag=&nPage=1
- 10. (2010) National Assembly of the Republic of Korea | National Assembly Legal Information System. In. cited
- 11.Unar-Munguía M, Santos-Guzmán A, Mota-Castillo P J, Ceballos-Rasgado M, Tolentino-Mayo L et al. (2022) Digital marketing of formula and baby food negatively influences breast feeding and complementary feeding: a cross-sectional study and video recording of parental exposure in Mexico. BMJ Glob Health.
- 12.Yeo J H, Kim E Y. (2022) Social policies and breastfeeding duration in South Korea: A survival analysis of the national data. Midwifery. 1, 103282.
- 13. (2022) . How the Marketing of Formula Milk Influences Our Decisions on Infant Feeding [Internet]. 1st ed. Geneva: World Health Organization; .
- 14.Seth M J. (2017) South Korea’s Economic Development, 1948–1996 [Internet]. Available from:https://oxfordre.com/asianhistory/view/10.1093/acrefore/9780190277727.001.0001/acrefore-9780190277727-e-271
- 15.Nam S J, Hwang H, Lee Y L. (2024) Comparative study of poverty dynamics and income structure: Pre and post COVID-19 impact on households with and without disabilities in South Korea. Disabil Health J. 17(2), 101580.
- 16.Bank World. (2024) [Internet]. [cited. Overview. Available from:https://www.worldbank.org/en/topic/poverty/overview 3.
- 17.Kim C I, Lee Y, Kim B H, Lee H S, Jang Y A.Development of supplemental nutrition care program for women, infants and children in Korea: NutriPlus. Nutr Res Pract. 3(3), 171-9.
- 18.Ajzen I.The theory of planned behavior: Frequently asked questions. , Hum Behav Emerg Technol 2(4), 314-24.
- 19.CDC. (2023) Breastfeeding Benefits Both Baby and Mom [Internet]. Available from:https://www.cdc.gov/breastfeeding/features/breastfeeding-benefits.html#print
- 20.Halpin S. (2019) World Breastfeeding Week [Internet]. Available from:https://news.nnlm.gov/region_7/2019/08/05/world-breastfeeding-week/
- 21.Modak A, Ronghe V, Gomase K P. (2023) The Psychological Benefits of Breastfeeding: Fostering Maternal Well-Being and Child Development. Cureus.
- 22.Smith A S, Tabbaa M, Lei K, Eastham P, Butler M J et al. (2016) Local oxytocin tempers anxiety by activating GABAA receptors in the hypothalamic paraventricular nucleus. Psychoneuroendocrinology. Jan;63: 50-8.
- 23.Georgescu T, Swart J M, Grattan D R, RSE Brown.. The Prolactin Family of Hormones as Regulators of Maternal Mood and Behavior. Front Glob Womens Health 2021, 767467.
- 24.Walter M H, Abele H, Plappert C F. (2021) The Role of Oxytocin and the Effect of Stress During Childbirth: Neurobiological Basics and Implications for Mother and Child. Front Endocrinol. 12, 742236.
- 25.Breastfeeding. (2023) socioeconomic status, and long-term postpartum weight retention. Int Breastfeed J. 18(1), 1.
- 26.Jarlenski M P, Bennett W L, Bleich S N, Barry C L, Stuart E A. (2014) Effects of breastfeeding on postpartum weight loss among U.S. women. Prev Med. Dec;69: 146-50.
- 27.Lambrinou C P, Karaglani E, Manios Y. (2019) Breastfeeding and postpartum weight loss. Curr Opin Clin Nutr Metab Care. 22(6), 413-7.
- 28.Nagel E M, Howland M A, Pando C, Stang J, Mason S M et al. (2022) Maternal Psychological Distress and Lactation and Breastfeeding Outcomes: a Narrative Review. Clin Ther. 44(2), 215-27.
- 29.Hoff C E, Movva N, Rosen Vollmar AK, Pérez-Escamilla R. (2019) Impact of Maternal Anxiety on Breastfeeding Outcomes: A Systematic Review. Adv Nutr Bethesda Md. 10(5), 816-26.
- 30.Borra C, Iacovou M, Sevilla A. (2015) New Evidence on Breastfeeding and Postpartum Depression: The Importance of Understanding Women’s Intentions. Matern Child Health J. 19(4), 897-907.
- 31.Feltner C, Weber R P, Stuebe A, Grodensky C A, Orr C et al. (2018) Breastfeeding Programs and Policies, Breastfeeding Uptake, and Maternal Health Outcomes in Developed Countries [Internet]. Agency for Healthcare Research and Quality (AHRQ);. Available from:https://effectivehealthcare.ahrq.gov/topics/breastfeeding/research
- 32.Pérez-Escamilla R, Martinez J L, Segura-Pérez S. (2016) Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Matern Child Nutr. 12(3), 402-17.
- 33.Perrine C G, Chiang K V, Anstey E H, Grossniklaus D A, Boundy E O et al. (2020) MMWR Morb Mortal Wkly Rep. Implementation of Hospital Practices Supportive of Breastfeeding in the Context of COVID-19 — United States 69(47), 1767-70.
- 34.Office of the Surgeon General (US), Centers for Disease Control and Prevention (US), Office on Women’s Health (US). The Surgeon General’s Call to Action to Support Breastfeeding [Internet]. Rockville (MD): Office of the Surgeon General (US); 2011 [cited 2025 Mar 3]. (Publications and Reports of the Surgeon General). Available from:http://www.ncbi.nlm.nih.gov/books/NBK52682/ .
- 35.Health World. (2018) Organization, United Nations Children’s Fund (UNICEF). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative [Internet]. Geneva: World Health Organization;. cited
- 36.Patil D S, Pundir P, Dhyani V S, Krishnan J B, Parsekar S S et al. (2020) A mixed-methods systematic review on barriers to exclusive breastfeeding. Nutr Health. 26(4), 323-46.
- 37.Bae S P, Lee W R, Hahn W H, Shin H J, Ahn Y M et al. (2022) Survey of Korean pediatrician’s perceptions of barriers to and improvements in breastfeeding. Clin Exp Pediatr. 65(11), 540-6.
- 38.Jeong Y. (2024) Academy of Breastfeeding Medicine in Korea. Termination of BFHI certification in Korea. Available from:https://bfmed.co.kr/re/sub/mbi_read.html?cate=1&idx=1053 .
