Abstract
Vision impairment and blindness remain a challenge in developing countries, especially in rural communities. Notwithstanding, VISION 2020 global initiative seeks to eliminate avoidable blindness by 2020. This community-based cross-sectional study aimed at determining the accessibility of ophthalmic services and barriers to its utilization in rural communities in the Upper Denkyira West District, Ghana. One-hundred and seventy participants from 5 randomly chosen rural communities in the district were included. Participants were interviewed using a structured questionnaire. Socio-demographic information, information regarding accessibility, utilization, and barriers to eye care services were obtained. Descriptive statistics were carried out using SPSS version 23. The Chi-squared test was employed to determine associations. P-values less than 0.05 at a confidence interval of 95% were considered significant. Only 21.8% of participants had had eye examination within the past 3 years, with over half of the examinations undertaken at screening grounds and health centres. Significant associations were found between ophthalmic services utilization and increasing age (p = 0.004), female gender (p = 0.027) and those who had a past history of eye problem(s) (p = 0.0010. The study found gross inadequate utilization of ophthalmic services mainly due to unavailable ophthalmic services in the rural district. Public health education and eye care interventions should prioritize and target rural populations.
Key Messages
This study found gross inadequate utilization of ophthalmic services mainly due to unavailable ophthalmic services in the rural district. Rural dwellers were thus compelled to resort to harmful eye care practices. Public health education and eye care interventions should prioritize and target rural populations
Author Contributions
Academic Editor: Min Zhao, Post-doctoral Research Associate, China
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Nana Yaa Koomson, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Several studies have reported blindness and vision impairment as major health problems in developing nations 1, 2, 3, 4. According to the World Health Organization (WHO), 90% of all persons with visual impairment live in developing nations 1. The problem is more alarming among rural populations 5, 6, 7. Amponsa-Achiano et al.2 found that 90.3% of participants of an outreach clinic in a rural Ghanaian district had at least a disorder in one eye. Also, the Ghana National Blindness and Visual Impairment Study by the International Agency for the Prevention of Blindness (IAPB) showed a 0.79% prevalence of blindness in rural areas of Ghana relative to 0.67% in urban areas 3. Although rural cocoa farmers in Ghana were reported to have very poor perception about their vision, they failed to utilize available ophthalmic services 4. Eighty-five percent of these rural farmers reported they had poor or very poor vision, yet only 31.9% on Snellen visual acuity examination were found to have poor vision (6/24 - 6/60) or very poor vision (≤ 3/60). The relatively higher burden of eye and vision disorders in rural communities poses a major challenge to the attainment of Vision 2020 goals 8. Chandrashekhar et al.9 found that state-owned hospitals in India which had eye care facilities were too distant away from the rural villages, a major reason why many rural inhabitants avoided or underutilized ophthalmic services. Similarly, Dhaliwal and Gupta 10 attributed the poor usage of ophthalmic services among people with cataract in rural India to lack of affordable transport. Inadequate eye care personnel, inadequate eye care facilities, and unaffordable ophthalmic services have been described as major setbacks in preventing and treating avoidable causes of blindness in Africa 5, 6, 7, 11, 12. Ntsoane and Oduntan 13 found that most of the hospitals and health care centres with eye care facilities were situated in urban centres. According to them, this was a notable hindrance to universal ophthalmic services utilization. Moreover, the unequal delivery of ophthalmic services among rural communities and urban centres has been suggested as key contributing factor to the overwhelming burden of blindness and visual impairment in rural regions 13. Ashaye et al. 14 reported that rural dwellers in Western Nigeria were underserved because a chunk of ophthalmic services in Western Nigeria was situated in urban areas. Consequently, inhabitants in these rural communities who had preventable and remediable ocular disorders were left unattended to. According to Silva et al. 15, the number of ophthalmic practitioners per million-population is nine times more in the richest countries than the poorest countries, an evidence that availability of ophthalmic services varies between countries in different regions of the world. By considering a nation, availability of ophthalmic services could differ from one region to another, districts and even between communities. For instance, the reported optometrist to population ratio in Ghana was 1:377,661 and that of ophthalmologist was 1:324,552, many of whom practiced in cities leaving rural dwellers underserved 11.
Many rural inhabitants are thus compelled to resort to alternate sources of eye care including herbal preparations and traditional practices which are potentially harmful 16. Another reported primary hindrance to ophthalmic services in rural regions is the poor road network linking rural communities to health centres 15, 17.
Robin et al.18 also reported poverty as a major drawback to the utilization of ophthalmic services in both developing and developed countries. Low economic activity among rural inhabitants renders them incapable of paying for the cost of health services in general. Disorders which could be remedied at the onset are left to deteriorate 5.
Several studies have also indicated under usage of ophthalmic services in rural areas even when they are available and accessible 19, 20, 21. Ntsoane and Oduntan 13 identified socio-demographic characteristics, lack of knowledge on blinding eye care conditions, lack of felt need and socio-cultural beliefs as causes of the poor usage of existing ophthalmic services.
The tendency of resorting to alternate ophthalmic practices in the midst of many ocular conditions coupled with the lack of proper ophthalmic services is very high 16.
While poor utilization of appropriate ophthalmic services contribute to high prevalence of visual impairment and blindness, studies on accessibility and usage of ophthalmic services have not focused much on rural areas in Ghana 11, 22, 23, 24
This study seeks to determine the accessibility, utilization and barriers to uptake of ophthalmic services among rural communities in the Upper Denkyira West District, Ghana.
Methods
Study Area and Design
This community-based cross-sectional descriptive survey was conducted in the Upper Denkyira West District, Ghana from December 2017 to March 2018. With a total population of 60,054, the district is entirely rural 25. The district was served by 12 Community Health Centres and 4 private-owned clinics. None of the healthcare facilities had an eye unit.
Participant Selection and Procedure
Adult population 18 years and older who had lived in the district for not less than 3 years and consented to partake in the study were included. A total of 170 participants were included in this study. The Epi-InfoTM software version 7 (Centre for Disease Control, Atlanta, Georgia, USA) was used to calculate the sample size using the following parameters: the target population (18 years and older) of 28,684 25; expected frequency of 32% 26; 7% confidence limits and 95% confidence interval.
Five communities were randomly selected. This was chosen on the basis of previous district-wide studies 26, 27. All communities (list obtained from the district assembly) were assigned a number label. Each number was written on equally sized pieces of paper and folded up into a bowl. The 5 communities: Breman-Brofoyedu, Domenasi, Besease, Maudaso, and Nkotumso were then drawn one after the other from the bowl.
Thirty-four participants each from the 5 randomly selected communities were chosen using a systematic random sampling. This was done by selecting every second person who reported to the outreach grounds in response to announcements that were made earlier in the communities.
Participants were interviewed using a structured questionnaire. Socio-demographic information, information regarding accessibility, utilization, and barriers to eye care services were obtained.
Data Analysis
Data collected were analysed using the Statistical Package for Social Science (SPSS) version 23 (SPSS Inc, Chicago, IL, USA). Descriptive statistics were carried out and the Chi-squared test was employed to determine associations. P-values less than 0.05 at a confidence interval of 95% were considered significant.
Ethical Consideration
The study was conducted in accordance with the tenets of the Declaration of Helsinki. The district authorities and authorities of the various communities were informed of the survey and their permission subsequently obtained. Informed consents were also gotten from study participants. Sufficient information was given to each participant to decide on partaking in the study or not. Participants’ anonymity and confidentiality were also kept.
Results
Socio-Demographic Characteristics
With a 100% response rate, participants’ mean age (±SD) was 46.86 (± 20.03) years; range 18- 84 years. Table 1 summarizes the socio-demographic characteristics of participants.
Participants’ Last Eye Examination (Figure 1)
Figure 1.Participants’ Last eye examination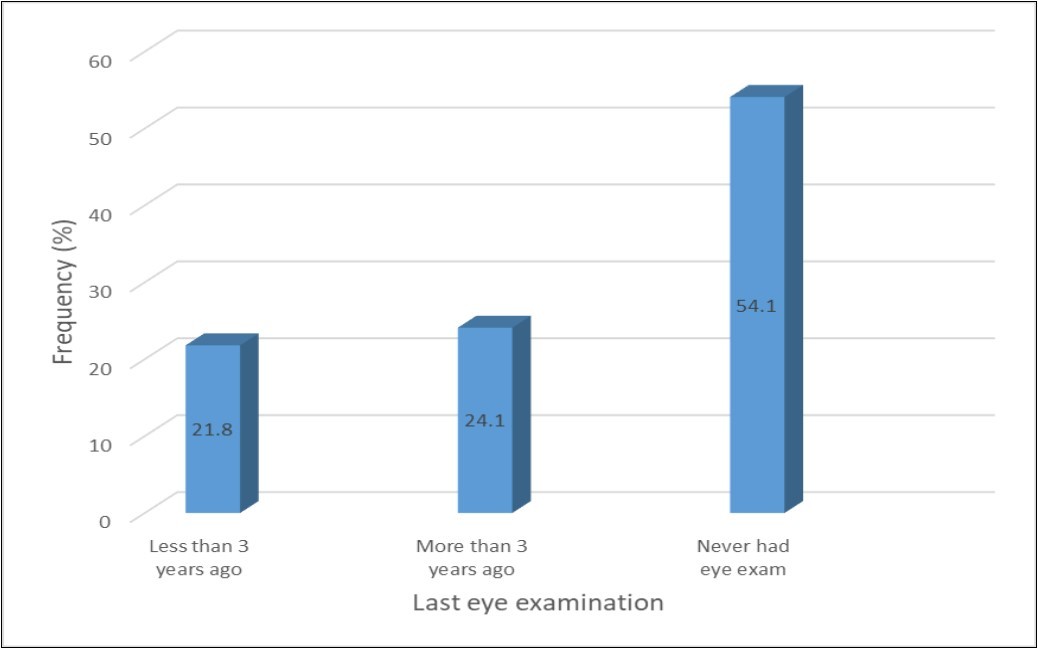
Access to Ophthalmic Services. (Table 2).
Participants past ocular problems and treatments sought (Table 3).
Influence of Socio-demographic Factors on Ophthalmic Service Utilization (Table 4).
Barriers to Ophthalmic Services Utilization
A total of 563 responses from 169 (99.4%) participants were obtained, giving a mean response of 3 per person (Table 5).
Table 1. Socio-demographic characteristics of participants| Variable | N (%) |
| Age group (years) | |
| 18 – 28 | 46 (27.1) |
| 29 – 39 | 20 (11.8) |
| 40 – 50 | 26 (15.3) |
| 51 – 61 | 33 (19.4) |
| 62 – 72 | 25 (14.7) |
| >72 | 20 (11.8) |
| Gender | |
| Male | 81 (47.6) |
| Female | 89 (52.4) |
| Highest educational level | |
| Never went to school | 33 (19.4) |
| Elementary | 92 (54.1) |
| Secondary | 35 (20.6) |
| Tertiary | 10 (5.9) |
| Employment status | |
| Employed | 92 (54.1) |
| Unemployed | 73 (42.9) |
| Retired | 5 (2.9) |
| Ethnicity | |
| Akan | 139 (81.8) |
| Ga-Adangbe | 1 (0.6) |
| Ewes | 7 (4.1) |
| Northern Tribe | 23 (13.5) |
| Religion | |
| Christianity | 159 (93.5) |
| Islam | 8 (4.7) |
| Traditional | 2(1.8) |
| Last Eye Examination | |||
| Less than 3 years ago N (%) | More than 3 years ago N (%) | Total (%) | |
| Place of last eye exam | |||
| Eye facility | 21 (26.9) | 14 (18.0) | 35 (44.9) |
| Health centre | 2 (2.6) | 9 (11.5) | 11 (14.1) |
| Outreach grounds | 14 (18.0) | 18 (23.1) | 32 (41.0) |
| Total | 37 (47.4) | 41 (52.6) | 78 (100.0) |
| Distance travelled to eye facility | |||
| Less than 5 km | 2 (5.7) | 1 (2.9) | 3 (8.6) |
| 5 – 8 km | 4 (11.4) | 3 (8.6) | 7 (20.0) |
| More than 8 km | 15 (42.9) | 10 (28.6) | 25 (71.4) |
| Total | 21 (60.0) | 14 (40.0) | 35 (100.0) |
| Time taken | |||
| Less than 30 minutes | 4 (11.4) | 2 (5.7) | 6 (17.1) |
| 30 minutes to 1 hour | 5 (14.3) | 4 (11.4) | 9 (25.7) |
| More than an hour | 12 (34.3) | 8 (22.9) | 20 (57.1) |
| Total | 21 (60.0) | 14 (40.0) | 35 (100.0) |
| Means of transport | |||
| Foot | 2 (5.7) | 2 (5.7) | 4 (11.4) |
| Public transport | 18 (51.4) | 11 (31.4) | 29 (82.9) |
| Private transport | 1 (2.9) | 1 (2.9) | 2 (5.7) |
| Total | 21 (60.0) | 14 (40.0) | 35 (100.0) |
Discussion
While only 21.8% of participants in this study had had their eyes examined within the past 3 years, more than half (54.1%) had never received an eye examination. Ebeigbe et al. 26 found a higher proportion (68%) of older persons (40-75 years) in rural Nigeria who had never received any eye examination. Also, Odutan and Raliavhegwa 28 in rural South Africa found 61% of a rural district populace who had never had their eyes examined. These studies however employed larger sample sizes which might have accounted for the relatively large percentages of non-usage of ophthalmic services.
Table 3. Participants’ past ocular problems and treatments sought| Past ocular history | ||||||
| Eye injury N (%) | Red eyes N (%) | Vision problemsN (%) | Red eyes And Vision problems N (%) | Eye injury and Vision problems N (%) | Total N (%) | |
| History of eye problem | ||||||
| Yes | 32(18.8) | 30(17.6) | 68 (40.0) | 6 (3.5) | 5 (2.9) | 141(82.9) |
| No | 29 (17.1) | |||||
| Treatment | ||||||
| Treated at an eye facility | 9 (5.3) | 3 (1.8) | 17 (10.0) | 1 (0.6) | 1 (0.6) | 31(18.2) |
| Used an eye drop obtained from a chemical shop | 13 (7.6) | 23(13.5) | 16 (9.4) | 5 (2.9) | 3 (1.8) | 60 (35.3) |
| Used herbal preparation | 5 (2.9) | 0 (0.0) | 8 (4.7) | 0 (0.0) | 1 (0.6) | 14 (8.2) |
| No treatment | 5 (2.9) | 4 (2.4) | 27 (15.9) | 0 (0.0) | 0 (0.0) | 36 (21.2) |
Although there are minor differences in reported levels of ophthalmic services utilization in rural areas, many are consistent indicators of inadequate utilization 11. Coincidentally, Ocansey24 found the same proportion (45.9%) of elderly participants (40 years and above) ever utilizing ophthalmic services in an urban Ghanaian region. While this was unexpected, it could possibly be because of reported barriers to uptake of available, accessible and affordable ophthalmic services 13. This seems to better explain the coincidence as 45.2% of participants in a Ghanaian urban community who had never checked their eyes were of the view that their eye problems were not bothersome 23.
In this study (table 4), about 82.9% of the participants indicated they had ever experienced at least one form of eye problem. About 40% indicated they had problems with vision. Yet, 15.9% of those who reported reduced vision received no treatment. In a Nigerian rural study, Ebeigbe et al. 26 found that rural dwellers do not see reduced vision as a problem until they can no longer perform their visual task. Again, this study found that non-prescription drops from chemical shops were used by 13.5% of the participants to manage red eye conditions. Herbal and/or traditional preparations were also common ways of treating eye injuries and red eyes. This was similar to the findings of Ovenseri-Ogbomo et al. 29 on ophthalmic services utilization in shanty areas of the Accra Metropolis (Ghana) where study participants between 18 and 80 years were found to use sea water and breast milk in managing some eye disorders. Again, the report of an urban study in Ghana was no different 23. Ntim-Amponsah et al. 16 found no significant difference (p=0.78) between patronage of alternate ophthalmic services and the regular ophthalmic services by participants of Akuapim South District, Ghana, revealing that easy access to alternate ophthalmic services and longer waiting hours at hospitals were the compelling factors. Of the 45.9% participants who had had an eye examination, there were more females (28.2%) than males. A significant association between ophthalmic services utilization and gender was thus found in this study (χ2 = 4.875; p = 0.027). Several studies also found significant associations between gender and ophthalmic services utilization affirming the fact that women seek more ophthalmic services than their counterpart 17, 26, 30, 31, 32, 33. Since older people are predisposed to many eye conditions, the relatively longer lifespan of women may be the reason why women access more eye care than men.
Table 4. Utilization of ophthalmic services by socio-demographic characteristics| Ever Had An Eye Exam? | p-value | ||
| Yes N (%) | No N (%) | ||
| Age (years) | |||
| 18-28 | 17 (10.0) | 29 (17.1) | 0.004* |
| 29-39 | 4 (2.4) | 16 (9.4) | |
| 40-50 | 16 (9.4) | 10 (5.9) | |
| 51-61 | 13 (7.6) | 20 (11.8) | |
| 62-72 | 13 (7.6) | 12 (7.1) | |
| >72 | 15 (8.8) | 5 (2.9) | |
| Gender | |||
| Male | 30 (17.6) | 51 (30.0) | 0.027* |
| Female | 48 (28.2) | 41 (24.1) | |
| Highest educational level | |||
| Never went to school | 20 (11.8) | 13 (7.6) | 0.179 |
| Elementary | 41 (24) | 51 (30.0) | |
| Secondary | 12 (7.1) | 23 (13.5) | |
| Tertiary | 5 (2.9) | 5 (2.9) | |
| Employment status | |||
| Employed | 40 (23.5) | 52 (30.6) | 0.326 |
| Unemployed | 37 (21.8) | 36 (21.2) | |
| Retired | 1 (0.6) | 4 (2.4) | |
| Ethnicity | |||
| Akan | 63 (37.) | 76 (44.7) | 0.078 |
| Ga-Adangme | 1 (0.6) | 0 | |
| Ewes | 6 (3.5) | 1 (0.6) | |
| Northern Tribe | 8 (4.7) | 15 (8.8) | |
| Religion | |||
| Christianity | 75 (44.1) | 84 (49.4) | 0.427 |
| Islam | 2 (1.2) | 6 (3.5) | |
| Traditional | 1 (0.6) | 2 (1.2) | |
| History of eye problem | |||
| Yes | 74 (43.5) | 67 (39.4) | 0.001* |
| No | 4 (2.4) | 14.7) | |
Also in this study, a statistically significant association (χ2 = 17.204; p = 0.004) was found between ophthalmic services utilization and increasing age. Kovai et al.19, Robin et al. 18, Schaumberg et al. 32have all reported positive associations. This could generally be due to the increased susceptibility to ocular problems as one ages. With the gradual decrease in vision, older people are more expected to seek ophthalmic care than young people who perceive eye problems as a disease of old age.
Although 74.4% of participants who have had eye examination had obtained at least elementary education, there was no significant association (χ2 = 4.909; p = 0.179) between highest educational level and ophthalmic services utilization in this study. This was contrary to Fotouli et al. 34 who reported a significant association between ophthalmic services utilization and highest educational level, asserting one was more expected to seek ophthalmic care when he or she is much educated. Fatouli et al. 34 believed that educated people seek ophthalmic services because they may have a better knowledge of their condition and also understand the implications of not seeking attention to their eye problems. Also, educated people mostly belong to the higher socioeconomic class, thus are more capable of bearing the total cost of ophthalmic services.
Again in this study, no significant associations were found for employment status (χ2 = 2.241; p = 0.326), ethnicity (χ2 (2) = 6.811; p = 0.078), religion (χ2 = 1.701; p = 0.427), and ophthalmic services utilization.
A statistically significant association was nonetheless found in this study between those who had a past history of eye problem(s) and ophthalmic services utilization (χ2= 14.500; p = 0.001). In rural Nigeria, Ebeigbe et al. 26 also found that people who had no or minor eye problems scarcely utilized ophthalmic services. This explains why people who found their eye problems unbearable more probable to utilize ophthalmic services as there was a need or reason to do so.
About 44.9% (table 2) of participants in this study who had had their eyes examined at an eye care facility did so outside the district. The remaining majority received their examination from outreach grounds and health centres. None of the clinics nor the community health centres had an eye care professional or an ophthalmic unit. This implies that non-eye care professionals attended to patients who presented with eye problems. For those who were seen at outreach grounds, they had to wait with their problems until luck shone on them for mobile eye clinics to come to their aid. This may be risky in cases of ocular emergencies. The few who travelled to eye care facilities travelled a distance of more than 8 km taking more than an hour (Table 2). Chatora and Tumusine 35 recommended that an individual accessing primary health care should not travel over 8 km distance and over 60 minutes time. It was in light of the poor access to primary health care that called for the Declaration of Alma-Ata in 1978 stating that access to primary eye care is fundamental human right.
The lack of any eye care facility in the Upper Denkyira West District was the major hindrance to eye care as 17.6% of all responses to barriers to eye care utilization indicated “there are no eye clinics around” (Table 5). Buchanan and Horwitz 36 also found unavailable eye care facilities and limited eye care personnel as the major barrier to ophthalmic services in rural Jamaica. According to Buchanan and Horwitz, the unavailable services accounted for more than 43% of the rural Jamaican populace who had never examined their eyes. Residents in the Upper Denkyira West District had to travel outside the district to seek eye care which could be inconvenient to make people consider their eye problems not too serious to demand intervention. Unaffordable cost of ophthalmic services, challenges with transportation, beliefs that eye problems were of a spiritual cause than medical, preference to herbal and/or traditional treatments were also reported barriers to ophthalmic services utilization in this study.
Table 5. Barriers to utilization of ophthalmic services among participants| Barriers | N (%) |
| There are no eye clinics around | 99 (17.6) |
| Nearest eye clinic too far away | 93 (16.5) |
| Can’t afford the cost of services | 79 (14.0) |
| My eye problems are not too serious | 74 (13.1) |
| Challenges with transportation | 63 (11.2) |
| Do not have health insurance | 51 (9.1) |
| Do not see the need to check my eyes because I have not had an eye problem Not old enough (18-28 years) to be having eye problems | 40 (7.1)33 (5.9) |
| Prefer herbal or traditional treatment My eye problems are of a spiritual cause than medical | 24 (4.3)7 (1.2) |
| Total | 563 (100.0) |
Also in this study, about 5.9% of indicated barriers to ophthalmic services utilization was the fact that they were not old enough (18 and 28 years) to be having eye problems.
Moreover, about 13.3% of the participants in this study indicated their eye problems were not too serious that needed attention. Red eyes and itching were considered by participants as “normal” in that, they could easily be remedied with over the counter eye drops.
Conclusions
This study found gross inadequate utilization of ophthalmic services mainly due to unavailable ophthalmic services in the rural district. Some rural dwellers were thus compelled to make use of potentially harmful eye care practices such as the use of non-prescribed eye drops and herbal preparations.
Notwithstanding, older persons, females, and participants who had a past history of eye problem(s) significantly utilized more ophthalmic services.
Recommendation
Public health education and eye care interventions should prioritize and target rural populations. These interventions could yield positive outcomes as many visual impairing and blinding eye conditions are avoidable.
Acknowledgements
We express our profound gratitude to the authorities of the Upper Denkyira West District Assembly, chiefs and residents of the district for their permissio this study.
References
- 1.Pascolini D, Mariotti S P. (2010) Global estimates of visual impairment.Br. , J Ophthalmol 96, 614-8.
- 2.Amponsa-Achiano K, Lartey S, Nti-Boateng C, Tetteh C. (2014) Visual Impairment and Types of Visual Disorders Among Attendees of an Outreach Clinic for Eye Care in Rural Ghana. , Med. J. Ghana 3, 3-6.
- 3.Kumah E K, Wiafe B, Owusu Baffoe I. (2017) . Ghana National Blindness and Visual Impairment Study. IAPB Available from: https://www.iapb.org/vision-2020/ghana-national-blindness-and-visual-impairment-study/ .
- 4.Boadi-kusi S B, Kumi-kyereme A, Awusabo-asare K, Ocansey S, Kyei S. (2013) Perceptions about Vision and Utilization of Eye Care Services among Cocoa Farmers in a Rural Community in. , Ghana.Int J Heal Res 6, 17-25.
- 5.Oduntan O O, Mashige K P, Hansraj R, Ovenseri-Ogbomo G. (2015) Strategies for reducing visual impairment and blindness in rural and remote areas of Africa.African Vis Eye Heal. 74, 1-5.
- 6.Wilson N, Couper I, E De Vries, Reid S, Fish T et al. (2009) A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas.Rur Rem Heal. 9, 1061-4.
- 7.Rabinowitz H, Diamond J, Markham F, Wortman J. (2008) Medical school programs to increase the rural physician supply: A systematic review and projected impact of widespread replication.Acad. , Med 83, 236-40.
- 8.Owsley C, McGwin G, Scilley K, Girkin C A, Phillips J M et al. (2006) Perceived Barriers to Care and Attitudes about Vision and Eye Care: Focus Groups with Older African Americans and Eye Care Providers.Investig Opthalmology Vis Sci. 47, 2797.
- 9.Chandrashekhar T S, Bhat H V, Pai R P, Nair S K. (2007) Coverage, utilization and barriers to cataract surgical services in rural South India: Results from a population-based study.Public Health. 121, 130-6.
- 10.Dhaliwal U, Gupta S K. (2007) Barriers to the uptake of cataract surgery in patients presenting to a hospital.Indian. , J Ophthalmol; 55, 133-6.
- 11.Ilechie A A, Otchere H, Darko- Takyi C, Hallady A C. (2013) Access to and Utilization of Eye Care Services in. , Ghana.Int J Heal Res 6, 7-15.
- 12.Naidoo K, Savage B, Westerfall B. (2006) Creating a sustainable spectacle delivery solution.Vision.
- 13.Ntsoane M, Oduntan O. (2010) A review of factors influencing the utilization of eye care services.S Afr Optom. 69, 182-92.
- 14.Ashaye A, Ajuwon A J, Adeoti C. (2006) Perception of blindness and blinding eye conditions in rural communities.JNatl Med Assoc;. 98, 887-93.
- 15.Silva J C, Bateman J B, Contreras F. (2002) Eye disease and care. in Latin America and the Caribbean.Surv Ophthalmol 47, 267-74.
- 16.Ntim-Amponsah C T, WMK Amoaku, Ofosu-Amaah S. (2005) Alternate eye care services in a Ghanaian district. , GhanaMedJ 39, 19-23.
- 17.Palagyi A, Ramke J, du Toit R, Brian G. (2008) Eye care in Timor-Leste: a population-based study of utilization and barriers.Clin Experiment Ophthalmol. 36, 47-53.
- 18.Robin A L, Nirmalan P K, Krishnadas R, Ramakrishnan R, Katz J et al. (2004) The utilization of eye care services by persons with glaucoma in rural south India.Trans Am Ophthalmol Soc. 102, 47-54.
- 19.Kovai V, Krishnaiah S, Shamanna B R, Thomas R, Rao G N. (2007) Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh. , South India.Indian J Ophthalmol 55, 365-71.
- 20.Malhotra R, Uppal Y, Misra A, Taneja D K, Gupta V K et al. (2005) Increasing access to cataract surgery in a rural area--a support strategy.Indian. , J Public Health 49, 63-7.
- 21.Lewallen S, Courtright P. (2000) Recognising and reducing barriers to cataract surgery.Community eye Heal. 13, 20-1.
- 22.Abdul-kabir M, Ehianata O, Kumah D Ben, Osae E A, Benjamin B B et al. (2016) . Pattern of Ophthalmic Services Utilization in the Asawase Constituency of Ghana .IOSR J Nurs Heal Sci 5, 35-8.
- 23.Ocansey S, Kyei S, Gyedu B, Awuah A. (2014) Eye care seeking behaviour: a study of the people of Cape Coast. , Metropolis of Ghana.J Behav Heal 3, 101.
- 24.Ocansey S. (2014) Utilization of Eye Care Services among Ghanaian Elderly Population: Evidence from a Peri-Urban Community.Ophthalmol Res An Int. , J 1, 89-101.
- 25.GhanaStatisticalService G. (2014) District Analytical Report. Upper Denkyira West District: Available from: http://statsghana.gov.gh/docfiles/2010_District_Report/Central/Upper%20Denkyira%20West.pdf.
- 26.Ebeigbe J, Ovenseri-Ogbomo G. (2014) Barriers to Utilization of Eye Care Services in Rural Communities in Edo State, Nigeria Ebeigbe.Borno Med. , J 11, 98-104.
- 27.Budenz D L, Barton K, J Whiteside-de Vos, Schiffman J, Bandi J et al. (2013) Prevalence of glaucoma in an urban West African population: the Tema Eye Survey.JAMA Ophthalmol. 131, 651-8.
- 28.Oduntan A O, Raliavhegwa M. (2001) An evaluation of the impact of the eye care services delivered to the rural communities in the Mankweng Health sub-district of the Northern Province.S Afr Optom. 60, 71-6.
- 29.Ovenseri-ogbomo G, Kio F, Afful O. (2011) Eye care utilisation among slum dwellers in the 414 greater Accra region. , Ghana.East Afr Med J 88, 4.
- 30.Morales L S, Varma R, Paz S H, Lai M Y, Mazhar K et al. (2010) Self-Reported Use of Eye Care among Latinos.Ophthalmology. 117, 207-215.
- 31.Fotouhi A, Hashemi H, Mohammad K. (2006) Eye care utilization patterns in Tehran population: a population based cross-sectional study.BMC. , Ophthalmol 6, 4.
- 32.Schaumberg D A, Christen W G, Glynn R J, Buring J E. (2000) Demographic predictors of eye care utilization among women.Med. Care38: 638-46.
- 33.Ng’etich A S, Owino C, Juma A. (2016) Utilization of trachoma eye care services in central division of Kajiado County. , Kenya.Int Res J Public Environ Heal 3, 32-46.
- 34.Fotouhi A, Hashemi H, Mohammad K. (2006) Eye care utilization patterns in Tehran population: a population based cross-sectional study.BMC. , Ophthalmol 6, 4.
Cited by (4)
- 1.Kakati Abhijit, Das Amarendra Kumar, 2022, , , 391(), 859, 10.1007/978-3-030-94277-9_73
- 2.Junior Obinwanne Chukwuemeka, Barrah Sharon, Kobia-Acquah Emmanuel, Titiati Perfect Emefa, Karikari Lucy Akua Afriyie, et al, 2025, Referral Pattern and Comanagement of Patients With Keratoconus in West Africa: A Survey-Based Study of Optometrists in Ghana and Nigeria, Eye & Contact Lens: Science & Clinical Practice, 51(2), 70, 10.1097/ICL.0000000000001139
- 3.Akpa Noah Emmanuel, Tenmang Panshak Elisha, Ramyil Alice Venyir, Mpyet Caleb Damilep, 2025, Patient satisfaction with ophthalmic outpatient services, Latin American Journal of Ophthalmology, 8(), 11, 10.25259/LAJO_39_2024
- 4.Ezinne NE, Ekemiri KK, Chukwuma I, Ojukwu CS, Mashige KP, et al, 2023, Utilization of Eye Care Services in an Underserved Community in Enugu State, Nigeria, Nigerian Journal of Clinical Practice, 26(1), 81, 10.4103/njcp.njcp_398_22
